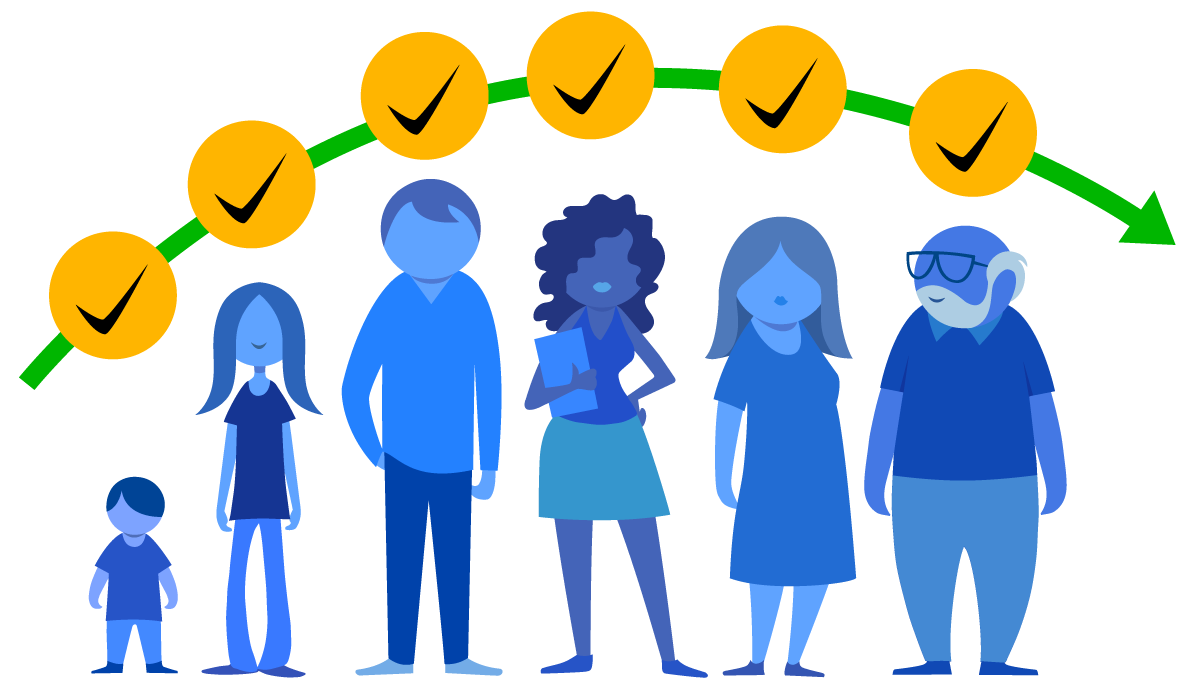
Immunization across the life course
The world is undergoing a profound demographic shift: there are now more persons older than 65 than children younger than 5. However, quality of life is not improving correspondingly.
As we age, our immune system weakens (immunosenescence) and leaves the body exposed to diseases to which it had gained immunity earlier. Also, chronic diseases exacerbate health outcomes when coupled with infections later in life.
The Life Course Approach (LCA) is a framework to help public health officials optimize health across the lifespan and identify key moments where health interventions can obtain maximum benefits for the well-being of individuals and communities.
A life course approach (LCA) to immunization states that persons should receive all recommended vaccine doses along their life course to reap the maximum benefits of preventing vaccine-preventable diseases (VPDs) at different ages, across generations, and within their communities.
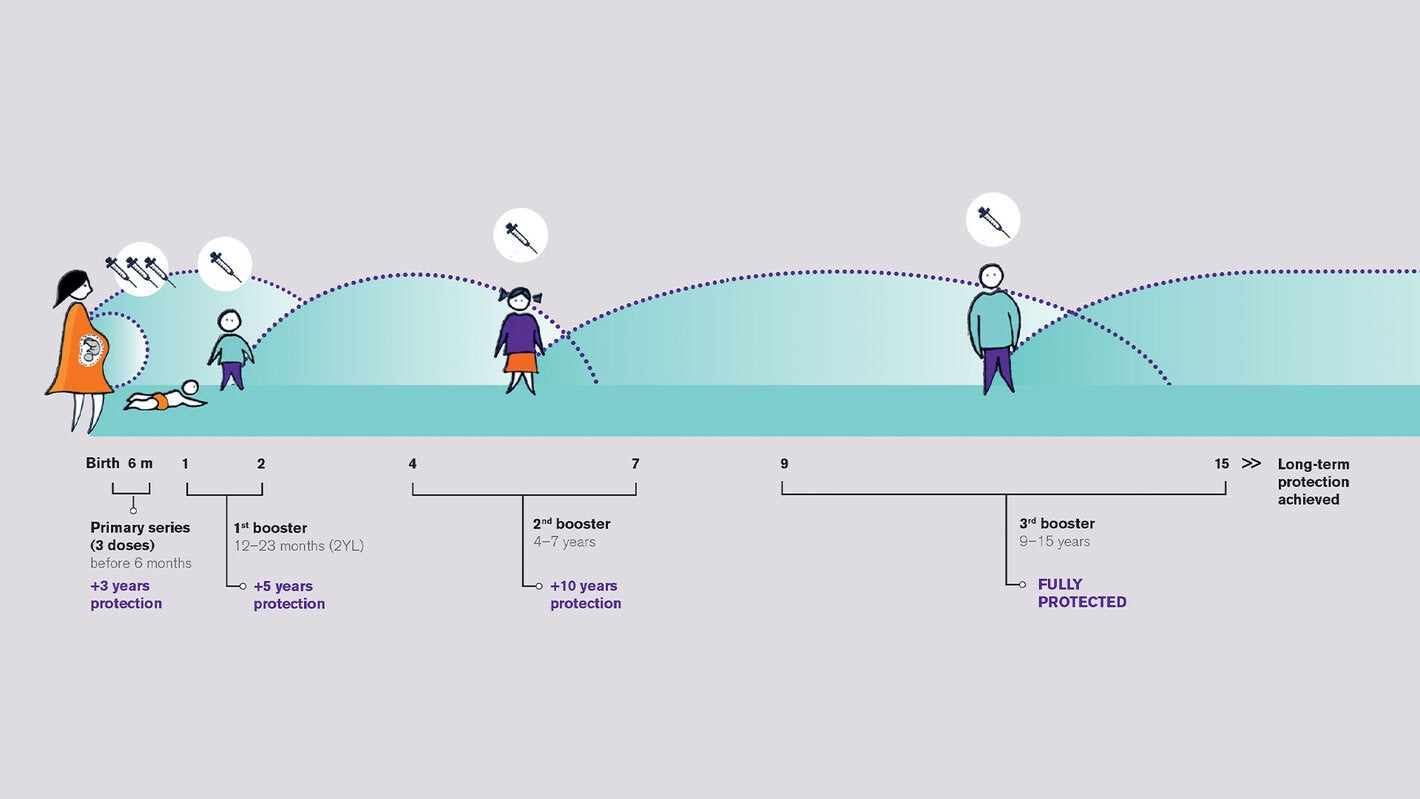
Example:
Tetanus is an acute infectious disease caused by spores of the bacterium Clostridium tetani. People who recover from tetanus do not have natural immunity and can be reinfected. Therefore, all persons should be vaccinated periodically to maintain protection. The WHO recommends that a person receive six doses of tetanus toxoid-containing vaccines. The primary series should begin at 6 weeks of age, with an interval of 4 weeks between doses. The three booster doses should be given at 12–23 months, at 4–7 years, and at 9–15 years. As the length of the life span continues to increase, countries can consider adding new booster doses to the national immunization schedule to protect older adults.
The LCA principles can be applied to national immunization programs. They can inform the development of vaccination platforms that:
- Administer vaccine doses at the time when the body is especially susceptible to a particular disease or when they are more cost-effective to prevent diseases at later life stages.
- Minimize the effects of immunosenescence by closing the most urgent immunity gaps for each age group.
- Improve health trajectories by integrating vaccination services with other age-appropriate health practices.
- Address health inequities and help achieve greater health outcomes with fewer resources.
Key messages
Health is a component of and a key resource for human development. Individuals and populations are affected by continuous interactions between themselves and the exposures and experiences of their environment – both over time and across generations. It is never too late to build health.
A Life Course Approach helps public health officials identify key moments and intersectoral activities where health interventions can be modified to obtain maximum benefits for the well-being of individuals.
By designing vaccination services that consider life trajectories, we can focus on closing immunity gaps to minimize the impact of disease, increase the body’s capacity to stay healthy across the stages of life, and reduce all-cause mortality rates in the population.
Address health inequities among individuals and within communities, and help achieve greater health outcomes with fewer resources over multiple generations.
A life course approach to immunization
Resources
Review what is already there
Many of the principles of the Life Course Approach are already embedded in national immunization programs of the Americas. Let’s review some examples where specific vaccines have clear advantages for the individual, the family and the community.
LCA considerations | Examples of protection against Vaccine Preventable Diseases |
|---|---|
| The primary series of a vaccine should be delivered at the sensitive/critical periods, while the person has a specific immunity gap against that disease. | The BCG vaccine is administered within the first 24 hours of life to protect newborns from tuberculosis while their neutrophil functions (i.e., one of the first immune cells to respond) fully develop. |
| In the life course approach, trajectories can reflect a decline or an improvement in health status. They are influenced by interdependent domains (e.g., work, school, reproductive life, migration) and factors (e.g., social, cultural, economic, political). | When administered before exposure to HPV – that is, prior to sexual intercourse – the vaccine can prevent infection and minimize the likelihood of developing precancerous and cancerous lesions later in life. |
LCA considerations | Examples of protection against Vaccine Preventable Diseases |
|---|---|
| Maternal immunization and infant health should be seen as a continuum, where one intervention positively impacts the well-being of two persons and builds intergenerational capacity to sustain immunity. | The Tdap vaccine during pregnancy was shown to be highly effective at preventing pertussis morbidity (69%–91%), hospitalizations (91%–94%), and death (95%) among infants. |
| A person’s health status is influenced by the generations that preceded them (e.g., parents, families, communities). By intergenerational transfer of traits, the same factors can impact their offspring. Therefore, health interventions must consider genetic links, social roles, and networks as influencers of health. | Breast milk includes maternal antibodies that can be shared with the baby and strengthen the child’s passive immunity. Breastfeeding is associated with better health outcomes in infancy and throughout adulthood. |
LCA considerations | Examples of protection against Vaccine Preventable Diseases |
|---|---|
| Prioritizing the vaccination of high-risk individuals who experience cumulative risk factors is cost-effective because it (a) reduces morbidity and mortality in these subgroups, (b) reduces the overall burden of disease in society and (c) reduces overall healthcare costs to treat cases of severe disease and its sequelae. | Vaccination against COVID-19 during the pandemic and in the post-pandemic period, where high-risk priority groups are prioritized. |
| Human agency is affected by social determinants (i.e., the conditions in which people are born, grow, work, live, and age). The life course perspective explores how health trajectories are shaped by the interaction between a person’s agency (i.e., individual thoughts and actions) and social determinants. | Vaccine hesitancy threatens to reverse progress made in tackling vaccine-preventable diseases. The reasons why people choose not to be vaccinated are complex and include complacency, inconvenience, and lack of confidence in the safety and effectiveness of vaccines. |
Also, vaccines already included in the national immunization schedule can contribute to the reduction of chronic or disabling health conditions by preventing the most common sequelae of VPDs.
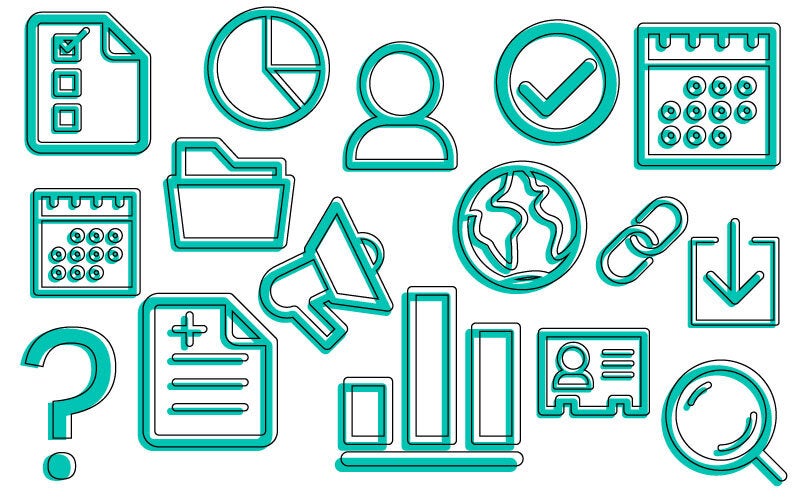
Consider what the national EPI needs to further implement the life course approach
We propose that any redesign of the immunization program in accordance with the principles of the LCA should focus on six elements of a national health system.
Advocacy: Promote expanded vaccination services that offer vaccine doses to all eligible persons according to their age and level of risk.
Financing: Ensure adequate and consistent financial resources to engage additional human resources and supplies. Such resources should be seen as a long-term investment given the economic and social benefit of immunizations.
Person-centered services: Create synergy between vaccination services for all age groups and other essential health services that are person-centered, age-appropriate and designed around users’ needs and demands.
Human resources: Communicate the positive impact of expanded immunization programs to public health officials, health administrators, health providers and vaccinators through trainings and supportive supervisory visits. Any encounter with the health system must become an opportunity to offer missing doses.
Information systems: Document the benefits of expanded immunization programs to assess the impact of vaccines on broader population health outcomes, healthcare services and public health priorities.
Equity: Establish targeted strategies to reach vulnerable populations. Outreach operations and cultural dialogues are well-documented activities that help reduce inequalities in vaccination coverage rates across the life course.
Related links

Reference documents
Immunization Agenda 2030 (IA2030) (global strategy)
IA2030 – Life-course & Integration (strategic priority document)
PAHO, CIM Plan of Action (under development)
PAHO, Building Health Throughout the Life Course. Concepts, Implications, and Application in Public Health (technical guidelines)
PAHO, Building Better Immunity: A Life Course Approach to Healthy Longevity (webinar)
PAHO, Building Better Immunity: A Life Course Approach to Healthy Longevity (technical guidelines)
PAHO, Building better immunity: A life course approach to healthy longevity (Appendix)
WHO, Reducing Missed Opportunities for Vaccination (MOV) (technical guidelines)
WHO, Working together: An integration resource guide for planning and strengthening immunization services throughout the life course (technical guidelines)
WHO, Global consultation on implementing vaccination checks at school (technical guidelines)
WHO, How to implement seasonal influenza vaccination of health workers (technical guidelines)
WHO, Leave no one behind: guidance for planning and implementing catch-up vaccination (technical guidelines)
WHO, Guidance on operational microplanning for COVID-19 vaccination (technical guidelines)
WHO, Implementation guide for vaccination of health workers (technical guidance)
WHO, Vaccinating older adults against COVID-19 (technical guidelines)
WHO, Behavioural and social drivers of vaccination: tools and practical guidance for achieving high uptake (technical guidelines)
PAHO, Maternal and Neonatal Immunization Field Guide for Latin America and the Caribbean (technical guidelines)
WHO, WHO recommendations for routine immunization - summary tables (technical guidelines)
WHO EURO, The life-course approach: from theory to practice: case stories from two small countries in Europe (technical guidelines)
Vaccines 4 All, Changing the Conversation on Adult Influenza Vaccination (consensus statement)
International Federation on Ageing, Messages Matter: A Spotlight on Influenza Vaccination Campaigns (technical document)
International Federation on Ageing, The Immunisation for All Ages Manifesto (document)
International Federation on Ageing, Improving Adult Vaccination Policy in Long Term Care Settings (technical report)
International Federation on Ageing, Evidence to Action: A review of the National Immunization Technical Advisory Groups (NITAGs) (technical report)
WHO, Improving the health and wellbeing of children and adolescents: guidance on scheduled child and adolescent well-care visits (technical guidance)