SUBMENU
Chikungunya is a viral disease transmitted to humans through by mosquitoes infected with the chikungunya virus. The mosquitoes involved in transmission are Aedes aegypti and Aedes albopictus.
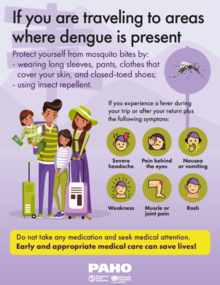
The most common symptom is an abrupt onset of fever, often accompanied by joint pain. Other symptoms include muscle pain, headache, nausea, fatigue, and rash. Severe joint pain usually lasts a few days but can persist for months or even years. Serious complications are uncommon, but atypical severe cases can cause long-term symptoms and even death, especially in older people and in children under one year old.
There is no vaccine or antiviral drug treatment for chikungunya. Treatment is focused on relieving the symptoms.
About chikungunya
- The word comes from the African Makonde language and means "bent over in pain."
- The disease was first described in Tanzania in 1952 and the virus was first isolated in Thailand in 1958.
- Chikungunya is not transmitted from one person to another. The virus needs a vector—a means of transportation: mosquitoes (Aedes aegypti and Aedes albopictus).
- The evidence available at this time demonstrates that Chikungunya virus infection produces lifelong immunity. The disease can be acquired only once due to the presence of antibodies that protect against future infection by the virus.
- The disease is endemic in the Americas, except in Canada, Chile, the United States and Uruguay.
- The treatment is symptomatic and in 98% of outpatient cases. Bed rest should be kept, preferably using mosquito netting. For pain and fever it is recommended to take Acetaminophen or Paracetamol, to control the fever. It is necessary to drink plenty of liquids (water, coconut water, soups, fruit juices, oral rehydration serum).
- There is currently no vaccine or specific drug against the virus.
- Cases of death from chikungunya are very rare and are almost always related to other existing health problems. Patients suffering from comorbidities or extreme health conditions in life have a greater risk of presenting serious forms and fatal outcomes due to this illness.
- Mothers who have chikungunya during pregnancy do not transmit the virus to their babies. However, there are documented cases of mother-to-child transmission when the mother has fever in the days immediately prior to delivery or during delivery.
About Aedes aegypti
Aedes aegypti is the vector that presents the greatest risk of arbovirus transmission in the Americas and is present in almost all countries of the hemisphere (except Canada and continental Chile). It is a domestic mosquito (that lives in and near houses) that reproduces in any artificial or natural container that contains water.
The mosquito can complete its life cycle, from the egg to the adult, in 7-10 days; adult mosquitoes usually live 4 to 6 weeks. The female Aedes aegypti is responsible for the transmission of diseases because she needs human blood for the development of her eggs and for her metabolism. The male does not feed on blood.
The mosquito is most active early in the morning and at dusk, so these are the periods of greatest risk of bites. However, females, who need to continue feeding, will seek a source of blood at other times. The female Aedes aegypti feeds every 3-4 days; however, if they cannot draw enough blood, they continue feeding each moment they can.
Aedes aegypti prefers to lay its eggs in artificial containers that contain water (drums, barrels and tires, mainly) in and around homes, schools and workplaces. Aedes aegypti eggs can withstand dry environmental conditions for more than a year: in fact, this is one of the most important strategies that the species uses to survive and spread.
To eliminate mosquitoes, the following actions are recommended: avoid collecting water in open-air containers (pots, bottles or other containers that can collect water) so that they do not become breeding sites for mosquitoes; adequately cover water tanks and reservoirs to keep mosquitoes away; avoid accumulating garbage, throwing garbage in closed plastic bags.
- PAHO/WHO provides advice and technical support to prenvent and control Chikungunya. This work is carried out on the basis of the Integrated Management Strategy for Arboviral Disease Prevention and Control, adopted by PAHO/WHO Member States in 2016 (CD55.R6).
- In 2008, PAHO/WHO Member States established a Dengue Laboratory Network of the Americas (RELDA) to strengthen technical capacities for dengue diagnosis. RELDA has now been expanded to include chikungunya and Zika fever and is now integrated by 40 laboratories in 35 countries in the Region.
- PAHO/WHO is supporting the development of an integrated epidemiological surveillance system model for dengue, chikungunya and Zika. This model integrates epidemiological, clinical, laboratory and entomological surveillance to generate standardized and timely information for decision-making. A technical document with guidelines for integrated epidemiological surveillance of dengue, chikungunya, Zika and other arboviruses will be published in 2024. Case definitions can be found here.
- Under the concept of collaborative surveillance, PAHO/WHO develops and makes virtual collaborative spaces (VCS) available to countries. Through the VCS, countries and PAHO collaborate in the real-time analysis of their epidemiological, clinical, laboratory and entomological data, as well as the generation of automated reports and bulletins.
- PAHO/WHO promotes a clinical technical cooperation package in the countries to strengthen national capacities for clinical diagnosis and case management of dengue, chikungunya, and Zika in the Region. This package includes technical documents and clinical guidelines, virtual self-learning courses, a regional virtual classroom to train trainers, and the setting up of national networks of clinical experts in arboviral diseases.
- PAHO/WHO promotes the strengthening of regional and national capacity for vector prevention and control through the implementation of the Plan of Action on Entomology and Vector Control 2018-2023. As part of this Action Plan, PAHO/WHO has developed several initiatives to improve entomological surveillance systems, as well as the monitoring and management of resistance to insecticides used in public health. A virtual course on Surveillance and Control of Vectors of Public Health Importance has also been created to train professionals in entomology. In addition, it promotes the implementation of a new model of interventions for the control of Aedes aegypti and provides support to countries for the rational deployment of new technologies and approaches for vector control.