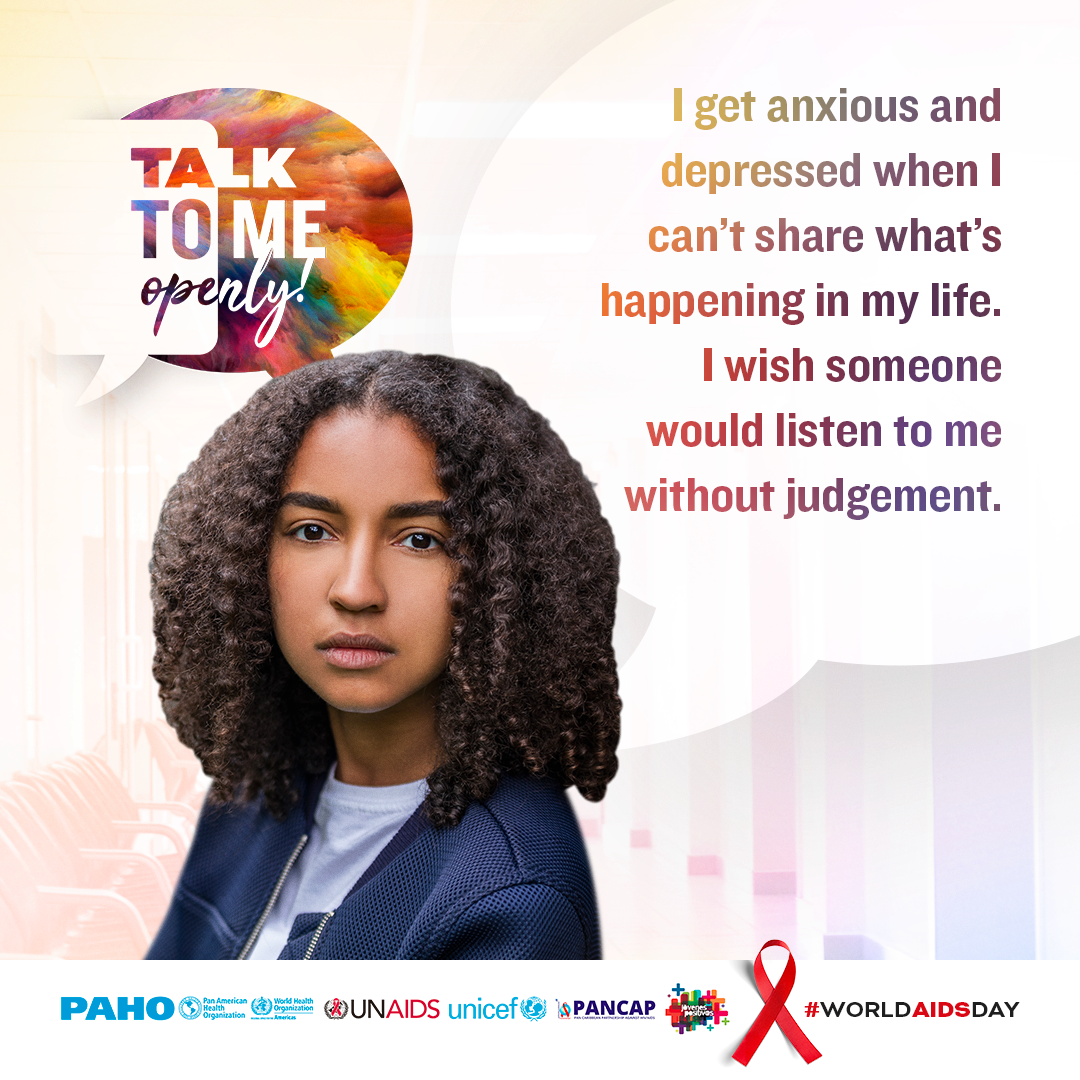
People living with HIV – including those from key populations – and their families and caregivers may have a wide range of mental health needs. Common mental health co-morbidities include depression and anxiety. Dementia and other cognitive disorders are also associated with longer-term HIV infection. HIV care settings can provide an opportunity for the detection and management of mental health problems among people living with HIV, including pre-existing mental health issues.
In addition to being disproportionately burdened by HIV, key populations experience higher rates of depression, anxiety, smoking, harmful alcohol use and alcohol dependence, other substance use and suicide as a result of chronic stress, social isolation, violence and disconnection from a range of health and support services.
Studies suggest that mental health disorders in people living with HIV may interfere with treatment initiation and adherence and lead to poor treatment outcomes. The presence of mental health co-morbidities may affect adherence to ART, due to forgetfulness or poor organization, motivation or understanding of treatment plans. Psychosocial support, counselling, appropriate drug therapies, and interventions such as case management may help to improve adherence to ART and retention in care.