10 September 2020
Facing up to NCDs
Honduras’ National Health Code (Decreto Numero 65-91, El Congreso Nacional) establishes the right of citizens to the assistance and care necessary for the promotion, conservation, recovery and rehabilitation of their health. Yet, access to this care remains an ongoing challenge, with more than four in ten of the country’s 9.2 million people living in rural areas.
Noncommunicable diseases (NCDs) are an enormous challenge to Honduras’s health systems. In 2016, NCDs represented more than two-thirds of all deaths in Honduras, and more than seven-in-ten premature deaths. Diabetes is a particular challenge, with more than half the population estimated to be living either without a diagnosis, or an appropriate treatment plan.
Despite the considerable health risks of diabetes, data on national prevalence and management remain extremely poor. Honduras does not have an updated population prevalence of diabetes nationally, with WHO estimating 7.2% of the population were living with diabetes in 2016.
60 SECOND READ
Fact: More than 650,000 people live with diabetes in Honduras, but the majority have either not been diagnosed, or do not have an adequate treatment plan.
Why it matters: A lack of information about diabetes treatment, glycaemic control and complications undermines the effective management of diabetes in the Honduran health system.
In practice: The project created a two-year National Plan and Monitoring Framework, agreed among key Honduran government institutions, to improve diabetes information systems in Honduras, and delivered new equipment to improve monitoring and surveillance.
As Dr Ricardo Rodríguez Buño, Pan American Health Organization (PAHO/WHO) explains, this is a big issue for patient care:
We estimate more than 650,000 Hondurans are living with diabetes. But the majority of them either have not been diagnosed, or do not have an adequate treatment plan. Strong surveillance and NCD registries are vital to change this.”
Concerningly, a partial population-based survey of diabetes, hypertension, and NCD risk factors conducted in the cities of Tegucigalpa and Comayagüela in 2009 found half of all people living with diabetes did not have an established diagnosis and treatment plan. In addition, the inconsistent data collection that does occur mainly addresses consultations or patient registration, without being able to determine that patient’s pathway.
Diabetes surveillance: lacking information and impairing decision-making
Timely health information, efficient system management and appropriate resourcing are all needed to enable decision-makers to assess the burden of NCDs in Honduras, and assign government resources accordingly. In this context, collecting, analysing and interpreting data on NCDs and their risk factors is vital.
However, to date Honduras has not had adequate systems to gather information on diabetes care. The information system used to collect diabetes data is inadequate to comply with the standards needed to inform decision-making by authorities and clinicians. Information systems are highly-fragmented, with few data-sharing processes in place.
As three examples:
- Honduras’s national Dialysis Control Program does not have a functional information system;
- Several dialysis clinics are outsourced to private providers using monopoly contracts, where records often only collect data on what sessions were provided, rather than clinical data;
- While the National Institute of Diabetics (Instituto Nacional del Diabético, INADI) has a digital information system, it is incomplete and does not routinely use electronic medical records.
Dr Laura Giacaman, director of epidemiology at the National Institute of Diabetics (INADI), explains these challenges:
Until 2018, we did not have a statistical or epidemiological surveillance unit. Since then we have been working to obtain data and information, but our resources are still very weak".
"It is vital to have an integrated information system that gives us information anywhere, anytime. This can permit us to make decisions for such important issues as human resources, medications, and actions. It also allows us to monitor and follow up on clinical management for the benefit of patients.”
There is a clear need to strengthen Honduras’s diabetes information system. By improving how information about diabetes is captured and communicated, not only will the population benefit, but the approach can also be a precedent for other institutions seeking to improve their management systems.
Fixing these challenges
A recent project, funded by the Government of Denmark, was granted to a coalition project led by the PAHO/WHO Country Office in Honduras, working with the Ministry of Health (Secretaría de Salud, SESAL) and INADI, and supported by other government institutions.
This coalition had a primary aim to create and agree a national plan for the improvement of the health information systems. To support this improvement, secondary aims of improving diagnostics and monitoring frameworks were also considered vital.
As a first step, activities were carried out to evaluate the available information related to diabetes in the healthcare system, and to improve the capacity and quality of information systems to assist clinical management.
This evaluation shone a light on several areas of need. In response, a framework for the effective surveillance and monitoring of diabetes and its complications was developed and validated by the working-group. This framework contains 21 indicators and 5 annexes, capturing data on aspects such as health outcomes, service productivity and performance, and quality of healthcare delivery.
Ing. José Ramón Pereira, director of the Information Management Unit (UGI), Ministry of Health, explains the value of this framework:
This framework is important because it allows us to advance a delay: we can now have standardized information from all health facilities as a first step to integrating these systems together.”
To progress this framework, a national plan for the improvement of health information on diabetes care for 2020-2024 was prepared. The plan set out ways to integrate NCD monitoring and surveillance into the existing health system.
It also finds key areas to improve. With technological strengthening as a particular area of concern, a procurement process was undertaken nationally to secure glucometers, biometric identification systems and computer equipment for health facilities.
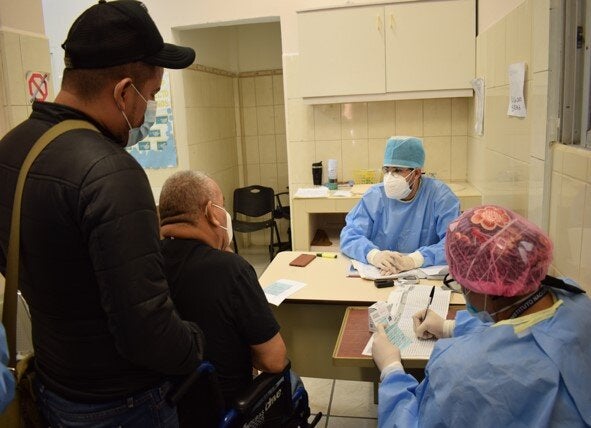
The national plan to improve health information for diabetes care will help reach people living with diabetes not previously diagnosed, improve patient care, and identify where equipment is needed. Credit: National Institute of Diabetics (Instituto Nacional del Diabético, INADI).
The result: stronger information systems, revitalised surveillance and working together towards one goal
Despite only beginning in April 2020, the project has allowed Honduras to lay the foundations for future action.
Most importantly, a National Plan has been created to develop information systems for diabetes and its complications. This roadmap includes milestones for development, such as strengthening dialysis registries, developing diabetic patient registries at central and regional levels.
While conducted in a very short time-scale, the National Plan will serve as a primer for larger structural developments across the country and rapidly improving diagnosis and monitoring capacity. It is hoped this work will create tangible improvements in both universal health coverage, and give diabetes patients the quality of care they deserve.
Importantly, grant funding has also enabled partners to achieve a technical agreement for the surveillance and follow-up of people living with diabetes, through a National Monitoring Framework.
As Dr. Karla Pavón, director of the Health Surveillance Unit (UVS), Ministry of Health summarises, this technical agreement ultimately means better care for people living with NCDs:
By generating unique information we can support decision-makers in a timely manner. Working with the health networks, we can move forward to detect the NCDs that are taking place all over the country."
Part of this technical agreement has included boosting the capacity for dialysis surveillance. The capacity of the national Dialysis Register is being doubled, through access to ten new biometric facilities that register a patient’s pathway. Ten new computers have also been placed in decentralised clinics, with software that enables data collection in a central database.
What’s more, people living with diabetes are also supported with 270 new glucometers, distributed to primary care and INADI health services to enable point-of-care glycaemic control.
The wide reach of the project has also been good for both patients and policy-making, as Dr. Alcides Martínez, Director-General of Integrated Networks of Health Services (RISS), Ministry of Health reflects:
… this project makes a great contribution, and will respond to patients’ needs while ensuring the optimal use of resources that the State invests in diabetes care”.
And with 21 indicators in the plan still to deliver on by 2024, there is much more to do.
Across the Global Week for Action on NCDs (7-13 September 2020), we are sharing stories from the field about why acting on NCDs is so important. These stories have emerged from a recent project funded by the Government of Denmark. Today's story was written by Dr Ricardo Rodriguez Buño and Mr Daniel Hunt. The authors give their acknowledgement and thanks to all partners involved in the project, and the experts who have provided their quotes.
Click on the following button form more stories