This roadmap responds to a proposal from the Pan American Health Organization and has been designed to support the countries of the Americas in the implementation of infection prevention and control (PCI) programs associated with health care, in accordance with the guidelines of the World Health Organization (WHO).
This proposal can be adapted to the local context and serve as a reference for countries with well-established IPC programs to verify compliance with the minimum requirements for IPC established by WHO, but also serves as a reference for countries with early-stage programs advanced in their development.
This roadmap is aimed at decision-makers, focal points for IPC programs, national, sub-national and local coordinators of these programs, as well as health personnel and the community in general.
ACRONYMS AND ABREVIATIONS
| AMR | antimicrobial resistance |
| HAIs | healthcare-associated infections |
| IHR | International Health Regulations |
| IPC | infection prevention and control |
| PAHO | Pan American Health Organization |
| PPE | personal protective equipment |
| SDGs | Sustainable Development Goals |
| SOP | standard operating procedure |
| WASH | water, sanitation, and hygiene |
| WHO | World Health Organization |
GOBERNANCE
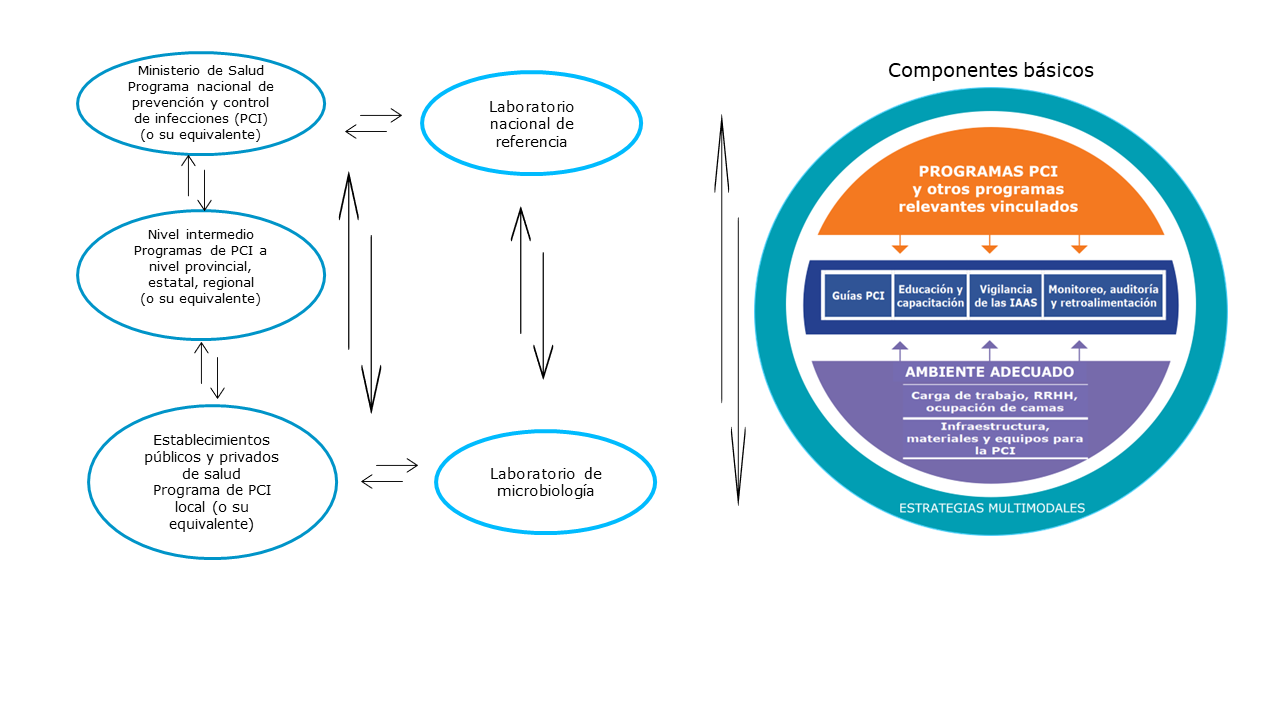
Figure 1 offers a governance structure for IPC programs and their core components (4). For the successful development of an IPC program, national1 and subnational2 authorities should coordinate their work with local authorities, and the coordination of core components includes all actors.
Figura 1. Esquema de la gobernanza para los programas para la Prevención y Control de Infecciones
_____________________________
Fuente: Publicado por OMS1 y adaptado por OPS/OMS, Programa especial de resistencia a los antimicrobianos.
-----------------------------------------------
(4) Guidelines on core components of infection prevention and control programmes at the national and acute health care facility level. Geneva: World Health Organization; 2016. License: CC BY-NC-SA 3.0 IGO.
(5) In this document, the national level refers to the Ministry of Health or its equivalent.
(6) In this document, the subnational level refers to the provincial, state, or regional level, or to the political or administrative structure that links the Ministry of Health to the health facility, in which a local IPC program already exists or will be implemented.
BASIC COMPONENTS
Core components of IPC programs
Since 2009, when WHO published the core components of IPC (updated in 2016) (4), there has been no doubt that IPC plays a fundamental role in the fight against AMR. This role has been recognized in both the International Health Regulations (IHR) and the Sustainable Development Goals (SDGs). In 2019, WHO established international minimum requirements for IPC, defined as the minimum requirements that should be in place at the national and health facility levels in order to provide the minimum necessary protection and safety to patients, healthcare workers, and visitors based on the WHO core components for IPC programs.
Most of the suggested indicators for evaluation of each component are based on yes/no answer, and all of them reflect compliance or non-compliance with the minimum requirements.
Considering the diversity of political-administrative structures and health systems in the countries of the Americas, this document highlights the importance of the subnational level in the coordination of IPC programs. While the national level (Ministry of Health or equivalent) in its regulatory role establishes which health policies are adopted in the country, it is the subnational level that facilitates and supervises local IPC programs in some countries.
The tables below describe the eight core components of IPC programs.
En referencia al título del Componente 1: "Otros programas vinculados"a
| National and subnational levels | Local Level | |
|---|---|---|
| Objective | Establish a national infection prevention and control (IPC) program | Establish a local IPC program |
| Minimum requirements | The national IPC program must have: • political and technical support to perform its functions; • well-defined objectives, functions, and activities; • a coordinator (focal point) trained in IPC, and other human resources; • a budget; • close coordination with the national reference laboratory. | Each sentinel(b) hospital or its equivalent must have: • a trained IPC coordinator with dedicated or assigned hoursc for coordination of the local IPC program; • a professional trained in IPC, with dedicated or assigned hours for local IPC program activities; • a budget for activities; • access to a microbiology laboratory; • technical and administrative support for implementation of activities. |
| Responsible | The Ministry of Health and the subnational level, through focal points who coordinate with the managers of relevant programs to establish synergies and seek the support of key partners to raise awareness about the national IPC program. | In each health facility with a local IPC program, the facility’s administrators and local program managers ensure compliance with the minimum requirements, as appropriate to the level of complexity of the health facility or institution. |
| Suggested indicatorsd | National level: • An IPC program is currently functioning, with work plans and an annual budget. National and subnational level: • An IPC coordinator (focal point) has been appointed, with time assigned to duties as program manager. • The appointed IPC coordinator(s) have received training in the prevention of healthcare-associated infections (HAIs). | Local level: • There is an IPC program with a dedicated budget and access to a microbiology laboratory. • There is an IPC coordinator who is trained in IPC and has assigned time(c) to accomplish the program manager functions. |
| Additional contributions on minimum requirements | The national IPC program focal point leads: • situation assessment of IPC core components and minimum requirements; • development of an action plan, including a budget; • preparation of norms, standards, indicators, and guidelines, • HAI surveillance; • compilation and analysis of information from the local level; • monitoring of progress of the action plan; • evaluation of the action plan; • feedback on the action plan; • dissemination of progress of the plan through periodic standardized reports. | The local IPC program coordinator leads: • development of standard operating procedures (SOPs); • proposal of local IPC indicators; • monitoring of compliance with local and national requirements; • surveillance and reporting of HAIs,e HAI outbreaks, and other important health-related events; • feedback from the local health team on achievement of goals and compliance with requirements; • dissemination of information on management results through periodic and standardized reports. |
------------------------------------
Notes:
(a) a For example, water, sanitation, and hygiene (WASH), antimicrobial resistance (AMR), International Health Regulations (IHR), budget and infrastructure, human resource management, and auditing
(b) Each country should define the local level at which the national IPC action plan will be implemented (e.g., sentinel hospitals, intensive care units, or other health services).
(c) The World Health Organization (WHO) recommends a ratio of 1 professional per 250 beds for local IPC (1).
(d) Prepared by the authors; copied or adapted from WHO documents. Instructions for the national infection prevention and control assessment tool 2 (IPCAT2) – Updated July 2017. Geneva: WHO; 2017. Available from: https://bit.ly/3iPDhsJ. Assessment tool of the minimum requirements for infection prevention and control programmes at the national level. Geneva: WHO; 2021. Available from: https://bit.ly/3F5myZO. Each country can also define its own indicators.
(e) e Routine notification (according to national requirements) of HAI outbreaks and other health-related events considered to be important (e.g., a previously undetected type of antimicrobial resistance or a change in the trend of the HAI curve).
| National level | Local Level | |
| Objective | Provide guidelines that promote patient safety and strengthen the fight against antimicrobial resistance (AMR). | Provide guidelines that promote patient safety and strengthen the fight against AMR. |
| Minimum requirements | Availability of evidence-based guidelines, approved by the Ministry of Health (or its equivalent), appropriate to the national context and reviewed every five years. | Existence of standard operating procedures (SOPs), updated and reviewed every five years, addressing at least the following topics: hand hygiene, decontamination of medical devices and patient care equipment, environmental cleaning, healthcare waste management, patient safety injections, protection of healthcare workers (e.g., post-exposure prophylaxis, vaccinations), aseptic techniques, triage of infectious patients, basic principles of standard precautions and transmission-based precautions. Appropriate use of personal protective equipment (PPE). In the case of second- and third-level health facilities, specific SOPs should also be in place, for example for the prevention of the most frequent healthcare-associated infections (HAIs) or the use of aseptic techniques in certain procedures. |
| Responsible | National infection prevention and control program (IPC). | Local IPC program |
| Suggested indicatorsa | • There are national guidelines and these are reviewed and updated at least every five years. | • SOPs based on national guidelines and adapted to the local context are reviewed and updated at least every five years and their compliance is periodically monitored. |
| Additional contributions on minimum requirements | The national IPC program focal point leads: • evaluation of new scientific evidence on IPC; • updates on the emergence of antimicrobial-resistant microorganisms and, in particular, those circulating for the first time in the country; • dissemination of information on the above points to all local IPC programs and other relevant programs. | The local IPC program coordinator leads: • updates and dissemination of SOPs to the entire health team. |
------------------------------------
Note:
(a) Prepared by the authors; copied or adapted from World Health Organization (WHO) documents. Instructions for the national infection prevention and control assessment tool 2 (IPCAT2) – Updated July 2017. Geneva: WHO; 2017. Available from: https://bit.ly/3iPDhsJ. Assessment tool of the minimum requirements for infection prevention and control programmes at the national level. Geneva: WHO; 2021. Available from: https://bit.ly/3F5myZO. Each country can also define its own indicators.
| National and subnational levels | Local Level | |
| Objective | Promote the education and training of health workers in infection prevention and control (IPC). | Promote education and practical training on IPC in the workplace, with the participation of patients and healthcare workers. |
| Minimum requirements | • Availability of a national policy on IPC education and training of health workers, validated by the Ministry of Health (or its equivalent). • Annual monitoring and evaluation of the effectiveness of IPC education and training. | • Education and training for health workers, professionals, technicians, and cleaners on the health facility’s standard operating procedures (SOPs) and IPC guidelines, according to their functions, at the start of their activities and then annually. • Creation and maintenance of a record of these activities. |
| Responsible | National and subnational IPC programs. | Local IPC programs. |
| Suggested indicatorsa | National and subnational IPC programs provide: • guidance and recommendations for training; • content and support for training of all health workforce; • a methodology and a monitoring schedule (e.g., at least once a year) to verify the effectiveness of training and education. | New workers are taught to apply SOPs and IPC guidelines. • Healthcare workers performing IPC-related functions receive specific annual education and training. • Guidelines on SOP supervision and compliance are properly implemented. |
| Additional contributions on minimum requirements | The national IPC program focal point leads: • creation and validation of a national policy on IPC education and training. | The local IPC program coordinator leads: • training in SOPs for new health staff members and annual training of permanent staff; • supervision of compliance with SOPs. |
------------------------------------
Note:
(a) Prepared by the authors; copied or adapted from World Health Organization (WHO) documents. Instructions for the national infection prevention and control assessment tool 2 (IPCAT2) – Updated July 2017. Geneva: WHO; 2017. Available from: https://bit.ly/3iPDhsJ. Assessment tool of the minimum requirements for infection prevention and control programmes at the national level. Geneva: WHO; 2021. Available from: https://bit.ly/3F5myZO. Each country can also define its own indicators.
| National and subnational levels | Local Level | |
| Objective | Establish a national active surveillance system for HAIs that is timely and that allows for comparative evaluation of the entire network of local infection prevention and control (IPC) programs. | Establish active local surveillance of HAIs and provide timely and sufficient information to guide interventions, detect outbreaks, and understand the national situation. |
| Minimum requirements | Creation of a multidisciplinary group (or committee) in charge of developing a strategic plan for HAIs surveillance, contributing to supervision of the surveillance system,a and monitoring IPC. | Local IPC program must be able to detect and report outbreaks, monitor HAIs trends in accordance with national guidelines and the local context, and provide timely and systematic reports to health facility authorities for decision-making. |
| Responsible | National and subnational IPC programs. | Local IPC program. |
| Suggested indicatorsb | • There is a strategic plan for HAIs surveillance (with a focus on priority infections according to the local context). • Standardized and periodic reportsc are prepared on the status of HAIs at the subnational and national levels. | • Standardized data on HAIs and antimicrobial resistance (AMR) are entered in (or submitted to) the national system monthly. • HAIs outbreaks are reported to health facility authorities and to the national and subnational IPC programs. |
| Additional contributions on minimum requirements | • The national IPC program focal point leads the preparation of reports, including: • The system: | The local IPC program coordinator leads: • preparation of reports on compliance (or not compliance) of the surveillance indicators established at the national and local levels; • dissemination of local and national reports. |
----------------------------------------
Notes:
(a) Ideally, an online system that allows data to be obtained, reviewed, and monitored in real time.
(b) Prepared by the authors; copied or adapted from World Health Organization (WHO) documents. Instructions for the national infection prevention and control assessment tool 2 (IPCAT2) – Updated July 2017. Geneva: WHO; 2017. Available from: https://bit.ly/3iPDhsJ. Asessment tool of the minimum requirements for infection prevention and control programmes at the national level. Geneva: WHO; 2021. Available from: https://bit.ly/3F5myZO. Each country can also define its own indicators.
(c) Periodicity is defined according to the local context and the requirements of national authorities. Semiannual or annual reports are suggested
(d) Selection of infections to be monitored is based on assessment of the national situation and on scientific evidence. In general, these are preventable infections that can cause epidemic outbreaks or high levels of mortality.
Multimodal strategies comprise several elements or components (three or more, usually five3), implemented in an integrated manner to improve a result and change behavior. They include tools such as kits and checklists developed by multidisciplinary teams, taking local conditions into account.
| National and subnational levels | Local level | |
| Objetive | Promote multimodal strategies, in accordance with national guidelines, that facilitate the implementation of infection prevention and control (IPC) programs. | Promote multimodal strategies that contribute to the prioritization of IPC interventions. |
| Minimum requirements | Adoption of multimodal strategies for the implementation of IPC programs, in accordance with national guidelines and standard operating procedures (SOPs) for IPC, coordinated by the IPC focal point. | Adoption of multimodal strategies to improve the implementation of standard precautions, as well as precautions to prevent infections associated with invasive procedures. |
| Responsible | National and subnational IPC programs. | Local IPC program. |
| Suggested indicatorsa | IPC focal points at the national and subnational levels are properly trained and know the scientific basis for program implementation, multimodal improvement strategies, and their application to IPC. IPC national and subnational program focal points are trained and competent in implementation science and multimodal behavior change strategies. Multimodal strategies are promoted by including the multimodal approach in the development of guidelines and courses for IPC education and training. | • Multimodal strategies are used to implement priority IPC interventionsb. • Adoption of preventive measures is monitored. |
| Additional contributions on minimum requirements |
| The local IPC program coordinator leads: • identification of people recognized as leaders or role models in the facility; |
-----------------------------------------
(a) Prepared by the authors; copied or adapted from World Health Organization (WHO) documents. Instructions for the national infection prevention and control assessment tool 2 (IPCAT2) – Updated July 2017. Geneva: WHO; 2017. Available from: https://bit.ly/3iPDhsJ Asessment tool of the minimum requirements for infection prevention and control programmes at the national level. Geneva: WHO; 2021. Available from: https://bit.ly/3F5myZO. Each country can also define its own indicators.
(b) At a minimum, interventions to improve hand hygiene, safe injection practices, decontamination of medical instruments and devices, environmental cleaning, and measures to prevent device-associated infections (1).
(c) For example, leaders in water, sanitation and hygiene (WASH), antimicrobial resistance (AMR), International Health Regulations (IHR), budget and infrastructure, human resource management, auditing, communications, universities, and research centers.
**************************************
(3) Components of multimodal strategies: 1) system change (availability of adequate infrastructure and supplies for IPC and good practices); 2) education and training of health workers and key actors (e.g., managers); 3) monitoring of infrastructure, practices, processes, results, and feedback on the data provided; 4) workplace reminders and communications; and 5) culture of changing or strengthening security in the facility.
| National and subnational levels | Local level | |
| Objetive | Establish a system to monitor, audit, and evaluate the action plan for infection prevention and control (IPC). | Establish a system to monitor, audit, and evaluate the IPC plan or activities. |
| Minimum requirements | Creation of a multidisciplinary group (or committee) for monitoring, auditing, and feedback on compliance with the goals, objectives, and activities of the action plan. The action plan includes minimum indicators, such as those related to hand hygiene, standard precautions, and transmission-based precautions. | The local IPC program helps to monitor national and local indicators and inform the corresponding levels regarding compliance, so that timely corrective measures are adopted. |
| Responsible | National and subnational IPC programs. | Local IPC program. |
Suggested indicatorsa | • Semiannual or annual report on the progress of the action plan and use of the allocated budget to carry out the activities specified in the plan. • National IPC indicators are integrated into the national monitoring system. | • Monitoring of information on compliance with hand hygiene rules, as well as feedback, are considered national-level core indicators, at least for reference hospitals. • Timely, periodic audit reports on the status of IPC activities and performance (e.g., feedback on data on compliance with hand hygiene and other processes) are provided to key stakeholders (particularly hospital management and senior administration) in order to take appropriate measures. |
| Additional contributions on minimum requirements | National and subnational IPC program focal points lead: • preparation of standardized semiannual or annual reports on the progress of the action plan; • review of the use of the budget allocated for IPC. | The local IPC coordinator leads: • maintenance and updating of timely, good-quality records on specific interventions; • coordination of evaluations, audits, and feedback on local interventions. |
------------------------------------
Nota:
(a) Prepared by the authors; copied or adapted from World Health Organization (WHO) documents. Instructions for the national infection prevention and control assessment tool 2 (IPCAT2) – Updated July 2017. Geneva: WHO; 2017. Available from: https://bit.ly/3iPDhsJ Asessment tool of the minimum requirements for infection prevention and control programmes at the national level. Geneva: WHO; 2021. Available from: https://bit.ly/3F5myZO Each country can also define its own indicators.
Components 7 and 8 were developed for implementation at the local level, with national-level coordination and support.
| Primary levela | Secondaryb and tertiary levelsc | |
| Objetive | Reduce overcrowding in health facilities and ensure good management of human resources. | Reduce the spread of infections in health facilities, avoiding overcrowding and work overload. |
| Minimum requirements | Development and implementation of guidelines on patient flow, triage and referral system, and consultation management. Sufficient human resources to carry out the activities in the action pland. | Availability of a system to manage the use of space, so that overall occupancy does not exceed the total number of beds planned for the facility. Determination of the standard number of beds for the health facility, with no more than one patient per bed, with at least 1 meter between the edges of the beds. Overcrowding is minimized and staffing is optimized by applying the same minimum requirements as for primary health care. |
Suggested indicatorsa | • Existen estrategias o directrices para reducir el hacinamiento. • Se evalúan los niveles de dotación de personal mediante estándares nacionales o internacionales o herramientas de evaluación ad hoc y se desarrollan planes de acción en función de los resultados. | • Staffing levels are assessed on the basis of national or international standards or ad hoc assessment tools, and action plans are developed based on the results. • Room design meets international standards for number of beds. • There are clear lines of responsibility for evaluation and response when the number of beds exceeds the facility’s total planned capacity (e.g., hospital administration or management is responsible). |
--------------------------------
(a) Primary level: In this document, this refers to hospitals at the first level of care that provide services in a few specialties (mainly internal medicine, obstetrics and gynecology, pediatrics, and general surgery) or simply general medicine. They have limited laboratory services (1).
(b) Secondary level: In this document, this refers to hospitals at the second level of care with 5–10 clinical specialties and a capacity of 200–800 beds.
(c) Tertiary level: In this document, this corresponds to tertiary care hospitals that have highly specialized staff and technical equipment (e.g. cardiology unit, intensive care, and specialized imaging units) and that provide clinical services differentiated by function. They can also carry out teaching activities. Their capacity varies from 300 to 1500 beds (1).
(d) To determine whether the available human resources are sufficient, it is recommended to use the World Health Organization (WHO) tool ‘Workload Indicators of Staffing Need (WISN)’. Available from: https://bit.ly/3IaQJ3z
(e) Prepared by the authors; copied or adapted from WHO documents. Instructions for the national infection prevention and control assessment tool 2 (IPCAT2) – Updated July 2017. Geneva: WHO; 2017. Available at https://bit.ly/3iPDhsJ Assessment tool of the minimum requirements for infection prevention and control programmes at the national level. Geneva: WHO; 2021. Available from: https://bit.ly/3F5myZO Each country can also define its own indicators.
| Primary levela | Secondary b and tertiary levelsc | ||
| Objetive | Have the necessary and appropriate infrastructure; water, sanitation, and hygiene (WASH) services; and infection prevention and control (IPC) materials and equipment for patient care. | ||
| Minimum requirements | Primary level:
| Secondary and tertiary levels: • A sufficient quantity of safe water is available for all necessary IPC measures and specific medical activities, including drinking. Piper water is available in the facility at all times, at least in rooms with high-risk patients (e.g. maternity ward, operating rooms, intensive care unit). • There are at least two improved, functional sanitation facilities that safely contain waste from outpatient wards, and 1 per 20 beds for inpatient wards. All of these must have supplies that facilitate menstrual hygiene. • Functional hand hygiene facilities are available at points of care, toilets, and service areas (e.g., decontamination unit). These should be as close as possible (e.g., less than five meters from toilets). • Sufficient and properly labeled containers are available and are used for separation of medical waste (as close as possible, e.g., less than five meters from where the waste is produced). Waste must be treated and disposed of safely by autoclaving, incineration (850°C to 1100°C), or burial in a lined and protected pit. • The facility’s design allows for adequate ventilation (natural or mechanical, as necessary) to prevent transmission of pathogens. • Sufficient and appropriate IPC supplies and equipment are available for all IPC practices, including standard and transmission-based precautions; and there is sufficient and appropriate electrical power to light clinical areas to provide safe, continuous care, at least in rooms with high-risk patients (e.g., maternity ward, operating rooms, intensive care unit). • A decontamination unit g is available, in accordance with minimum requirements. • There are suitable individual isolation rooms, or at least one room to group patients with similar pathogens or syndromes if the number of isolation rooms is insufficient. | |
| Suggested indicatorsh | All levels: • Water services are available at all times and in sufficient quantity for all uses.i For secondary and tertiary levels, the following indicators also apply: • There is water, soap, or alcohol-based hand sanitizer at all point-of-care stations (yes; in some, but not in all = no). | ||
-----------------------------------
(a) Primary level: In this document, this refers to hospitals at the first level of care that provide services in a few specialties (mainly internal medicine, obstetrics and gynecology, pediatrics, and general surgery) or simply general medicine. They have limited laboratory services for general (non-specialized) analysis (1).
(b) Secondary level: In this document, this refers to hospitals at the second level of care with 5–10 clinical specialties and a capacity of 200–800 beds (1).
(c) Tertiary level: In this document, this corresponds to tertiary care hospitals that have highly specialized staff and technical equipment (e.g., cardiology, intensive care, and specialized imaging units) and that provide clinical services differentiated by function. They can also carry out teaching activities. Their capacity varies from 300 to 1500 beds (1).
(d) Includes hand hygiene, environmental cleaning, laundry, and decontamination of medical devices.
(e) This should include soap, water, and disposable towels (or, if unavailable, clean reusable towels) or alcohol-based hand sanitizer (1).
(f) For example, brooms and other utensils for floor cleaning, detergent, disinfectant, PPE, and sterilization (1).
(g) An exclusive space or area to decontaminate medical devices for reuse (1).
(h) Prepared by the authors; copied or adapted from World Health Organization (WHO) documents. Instructions for the national infection prevention and control assessment tool 2 (IPCAT2) – Updated July 2017. Geneva: WHO; 2017. Available from: https://bit.ly/3iPDhsJ Assesment tool of the minimum requirements for infection prevention and control programmes at the national level. Geneva: WHO; 2021. Available from: https://bit.ly/3F5myZO Each country can also define its own indicators.
(i) For example, hand washing, drinking, personal hygiene, medical activities, sterilization, decontamination, cleaning, and laundry (1).
(j) For example, pumping and boiling water, sterilization and decontamination, incineration or alternative treatments, electronic medical devices, general lighting in areas where healthcare procedures are performed (to ensure safe provision of services), and lighting in bathrooms and showers (1).
NEXT STEPS
The core components of IPC should be implemented with a phased approach, beginning with selected sentinel hospitals or health facilities, and subsequently including all health facilities in the country.
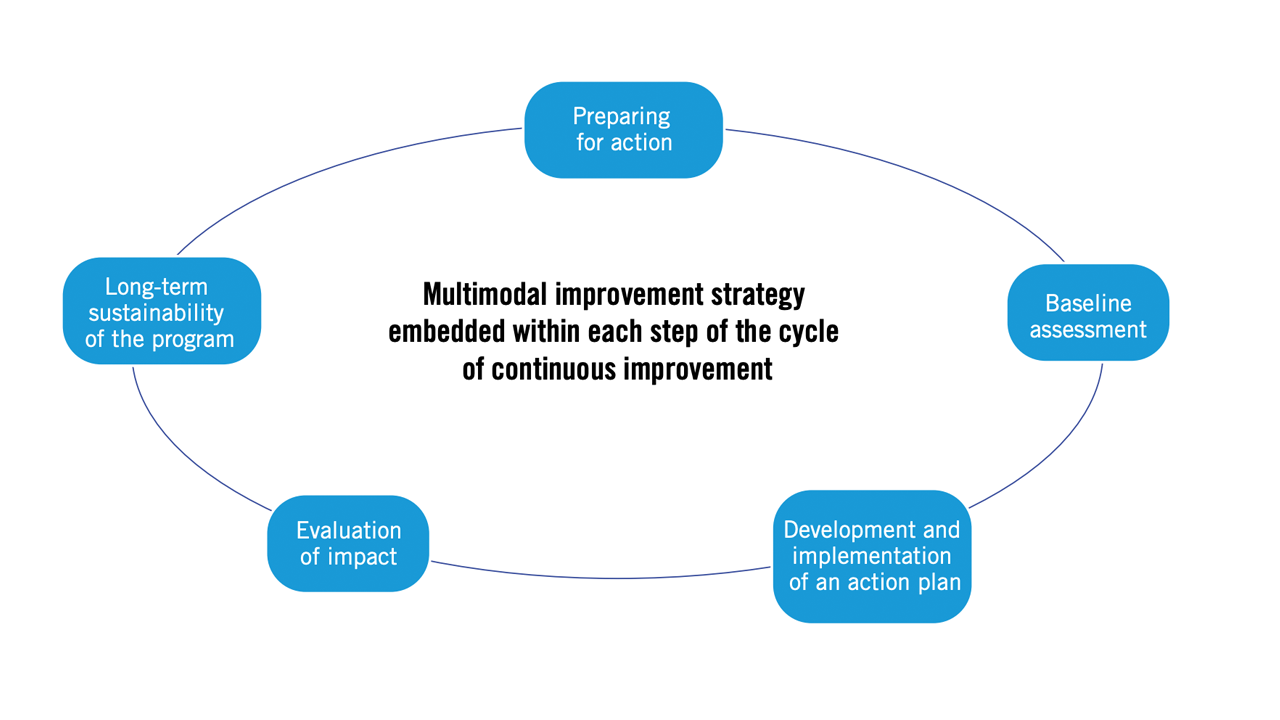
To facilitate the process of implementing or improving IPC, WHO proposes the five-step cycle shown in Figure 2.
The cycle begins with data collection, including background information and everything necessary for an accurate baseline assessment of the current situation and activities at the local level, determining the strengths (minimum requirements that are met) and weaknesses (requirements not met). Next, it is necessary to develop an action plan that takes into account local situation and available resources, and that prioritizes the key components for initial implementation. The next step is to evaluate short- and medium-term impacts to adjust the plan in order to ensure its long-term sustainability. The cycle is periodically repeated, and appropriate adjustments are made.
Source: The authors, based on: World Health Organization. Minimum requirements for infection prevention and control. Geneva: WHO; 2019. Available from: https://bit.ly/3XSDjjz.
REFERENCES
(1) Minimum requirements for infection prevention and control. Geneva: World Health Organization; 2019. License: CC BY-NC-SA 3.0 IGO.
(2) OMS. The role of infection prevention and control in preventing antibiotic resistance in health care. Geneva: World Health Organization; 2017. Licence: CC BY-NC-SA 3.0 IGO.
(3) Global report on infection prevention and control. Geneva: World Health Organization; 2022. License: CC BY-NC-SA 3.0 IGO.
(4) Guidelines on core components of infection prevention and control programmes at the national and acute health care facility level. Geneva: World Health Organization; 2016. License: CC BY-NC-SA 3.0 IGO.
SUGGESTED RESOURCES
- Handle antibiotics with care in surgery.
- Your 5 Moments for Hand Hygiene.
- Infection prevention and control28.
--------------------------