The 28 Days... Time to Care and Love campaign is a joint initiative of PAHO and its Latin American Centre for Perinatology (CLAP) that seeks to raise awareness regarding the importance of newborn care and provide relevant and evidence-based information on the subject. These two goals designed to provide quality care, contribute to the reduction of neonatal mortality rates, and increase awareness on the need for action in situations requiring specific interventions.
The campaign aims to increase the knowledge, skills and self-confidence of mothers, families and caregivers of newborns, and raise awareness about the importance of good newborn care practices and encourage assertive decision-making to reduce neonatal mortality among health professionals.
In the first hour after birth, babies have the ability to initiate breastfeeding on their own. At birth, after gently drying them, newborns are placed face down directly on the skin of the mother's abdomen and breast, without contact interferences. Skin-to-skin contact during the first hour of life makes it easier for the baby to maintain its body temperature, recognize sounds (including voices), calm down and reach the goal that smell and sight indicate: the mother's breast.
In this position, and given the time needed, they develop an activity that leads them to start sucking at the breast approximately one hour following birth. It is extremely important to allow them to start breastfeeding as soon as they show signs of being ready, without forcing them, and not to interrupt this contact until the colostrum intake has been completed. Breastfeeding is installed from the first postnatal hour.
It is recommended to initiate breastfeeding within the first hour following birth and to give the baby the necessary time of skin-to-skin contact with the mother. It is important not to interrupt this contact until the colostrum intake is completed.
Body temperature is a key issue when providing initial baby care. Although cold hands and feet are common in healthy newborns, this does not necessarily mean they are feeling cold.
Permanent closeness with the mother encourages skin-to-skin contact, which in turn helps to keep the newborn’s temperature stable. It is advisable to delay the first bath 24 hours following delivery and avoid air currents in the environment where the newborn is placed. Clothing should be in agreement with room temperature, although it is necessary to add one or two more layers as compared to what an adult would wear together with a cap.
Cold hands or feet are common in newborns but this does not mean they are feeling cold. Measures such as skin-to-skin contact with the mother and delaying the first bath 24 hours contribute to keep the body temperature stable.
Vaccines stimulate the body's defense system to protect the individual against subsequent infection or illness. It is important to vaccinate all children on time. The vaccination schedules include many different vaccines to be applied during childhood and even adult life.
Vaccines not only prevent diseases and the corresponding disabilities, they also contain their spread. They are an instrument of individual and collective protection that impacts on the whole of society.
The mother’s milk production increases during the first hours and days following delivery with the stimuli of the baby at the breast. Colostrum secretion starts during the first minutes following delivery. It is a yellowish fluid of high nutritional value with very unique and appropriate benefits during this period. Its intake is extremely important for newborns.
It is essential that newborns only receive mother's milk and only suck at the mother's breast. When babies ingest other fluids or foods they feel less need to breastfeed, their demand to be breastfed decreases and thus milk production in the mammary gland falls. Sucking objects other than the nipple may confuse them.
Breastmilk is adapted to the baby's needs, and is initially known as colostrum. Exclusive breastfeeding is recommended.
A baby's umbilical cord should be kept clean and dry. No substances or objects are to be placed in this area. If moisture, odour or redness on the skin of the umbilical cord is observed when changing the nappy, you should seek advice.
The skin of newborn babies, the amniotic fluid and the vernix or sebaceous lining that covers them contain substances to protect them against infection. It is recommended not to bathe newborns until at least one day following birth and not to apply any products or perfumes to the skin.
The nappy area may be wiped with calcareous oil, which should not be removed after cleansing.
The relationship with the health institution where the baby was born continues following discharge with outpatient check-ups, office visits to confirm the newborn remains healthy and breastfeeding has been established appropriately.
Some conditions typical of the first days of life should be monitored to ensure the baby’s well-being: possible jaundice, weight gain and the umbilical cord condition. If any treatment is required, outpatient appointments shall be offered in a timely manner, in order to avoid harmful consequences for the baby. Most importantly, medical office visits offer a chance to clear any possible doubts that could arise during the first days at home. This is why it is a priority to attend appointments as agreed with the health team.
Conditions that may arise during the first days of life are monitored in outpatient appointments to ensure the newborn remains healthy. It is the right time to clear up any possible doubts with the health team. Attending the scheduled appointment is a priority.
Correct hydration of the mother is very important after the baby is born. The food the mother eats does not reach the milk she supplies to the baby.
A varied and healthy diet that contributes to well-being and prevents digestive discomfort facilitates availability for breastfeeding on demand.
Correct hydration of the mother following birth is extremely helpful for breast milk production. A healthy diet generates well-being and facilitates the availability to breastfeed.
In addition to health care, birth registration is essential in the first days of newborns. Registering the birth is the proof of the existence of a person in society and provides an identity to individuals by granting them name, surname, date of birth, sex and nationality. Identity is one of the fundamental rights of the human being, it characterises and distinguishes each individual as a unique being.
Once the identity has been obtained, the individual will be able to benefit from the other rights they are entitled to. It is advisable to register the birth during the stay in the maternity ward. When is not possible to access the civil registry in the institution where the baby was born it is very important to request the necessary information to enable registration as soon as possible before leaving the place.
In addition to providing health care it is necessary to register newborns and it is a right. Birth registration shall be done during the maternity stay; when not feasible it is necessary to request the corresponding as soon as possible.
Prolonged skin-to-skin contact of new-borns with their mother during the first postnatal hour favours the initiation of breastfeeding and subsequent support. After birth, the newborn is able to initiate breastfeeding on his or her own. In order to promote this ability the recommendation is to first dry them carefully and place them directly on the mother’s skin of the mother's torso as soon as possible. This makes it easier for them to maintain their body temperature, reach the breast and establish lactation. To accomplish this, babies need approximately 45 minutes to two hours, during which it is essential to avoid interrupting direct contact with the mother and to allow them to start sucking when they show signs they are ready, without pressing them to do so.
Step 4 of the Mother and Child Friendly Hospital Initiative is allowing close and uninterrupted contact during the first postnatal hour.
Initiating breastfeeding in this way facilitates its successful establishment and subsequent duration.
Babies born without complications should be placed in skin-to-skin contact with their mothers immediately following birth to prevent hypothermia and initiate breastfeeding.
In all term and preterm newborns wait the clamping the umbilical cord (1 to 3 minutes after birth, or until it stops beating) has both short and long term effects on life. Delay in clamping of the umbilical cord allows the transfusion of blood from the placenta to the newborn, which in turn improves their iron store and contributes to meet the requirements of this micronutrient during the first six months. These requirements are high during the first two years of life due to their rapid growth rate throughout this period.
During this period, in addition to the iron provided by breastfeeding, they require iron from their iron deposits.
Iron deficiency anaemia in infants and children during their first years of life, may increase the probability of developmental delay and decrease their performance at school. This is why delayed clamping of the umbilical cord is one of the essential care-measures in newborns.
Skin-to-skin contact at birth and timely clamping of the umbilical cord are health team interventions with long-term effects: they favour the onset of breastfeeding and the baby's iron store.
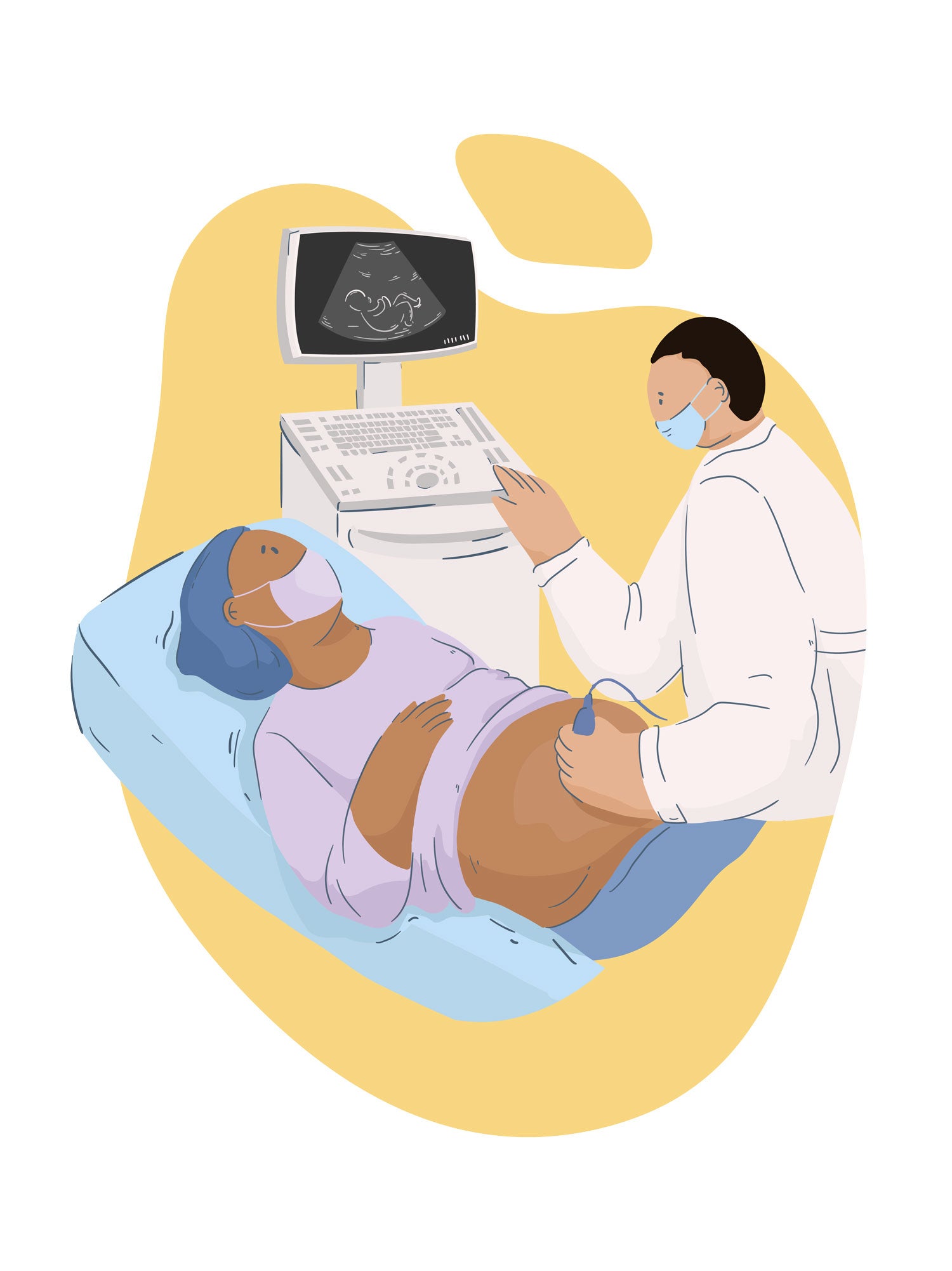
Different specific tests can diagnose diseases that, if treated immediately, can prevent serious consequences. These tests conducted after birth and before discharge from the care centre are known as neonatal screening tests and may serve to diagnose neurometabolic or structural diseases such as congenital heart defects or hip dislocation.
Early disease identification enables the correct treatment and prevention of important disabilities Prevention, timely diagnosis, and specific treatment may substantially contribute to reduce the burden of mortality and morbidity due to early conditions that have lifetime consequences for infants. Many countries have specific programs and legislation in this regard which determine the number and type of diseases evaluated. PAHO is developing guidelines providing evidence regarding tests and their effectiveness.
Why is screening at birth important? Because diseases identified early on may be treated or corrected thus preventing major disabilities and reducing mortality in newborns.
Some babies do not breathe or cry spontaneously at birth. In this situation, when newborns are not vigorous, the initial recommendation is to perform manual stimulation. For the reception of non-vigorous newborns in special situations, or when manual stimulation is not enough, the Basic Newborn Resuscitation Guidelines contain recommendations for specific treatment for each individual vitality state of non-vigorous newborns.
Manual stimulation is recommended for initial neonatal resuscitation in babies who do not cry spontaneously at birth. Other specific treatments for non-vigorous newborns are established in Evidence-based guidelines.
After birth, immediate skin-to-skin contact helps maintain the newborns’ temperature as they transition to life outside the uterus, while enhancing the mothers’ secretion of colostrum and creating an environment conducive to the onset of breastfeeding.
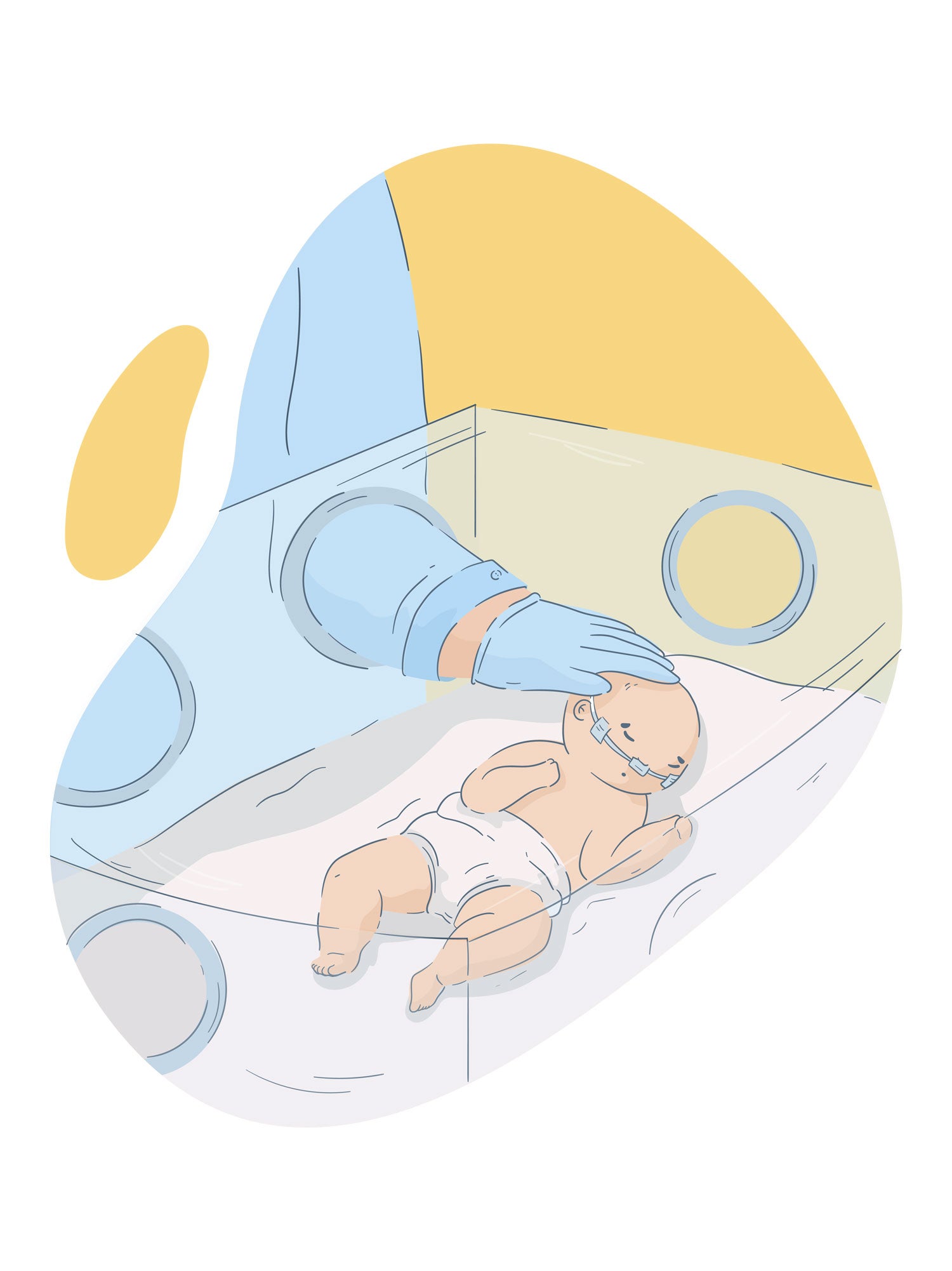
Like full-term newborns, premature newborns are entitled to beneficial skin-to-skin contact with their mother immediately after birth. This recommendation also applies to babies throughout their stay in the intensive care as long as they are clinically stable.
In premature infants, skin-to-skin contact during the hospitalization period may be implemented continuously round the clock. If unfeasible, it can be done intermittently, as often as possible.
When practiced throughout the hospitalization period, skin-to-skin contact is associated with:
A. Decreased neonatal mortality up to the first year of life.
B. Higher rates of exclusive or partial breastfeeding.
C. Higher and steeper weight-gain curves than those of preterm infants kept in incubators.
D. Optimized bonding.
Preterm infants, like term infants, benefit from skin-to-skin contact immediately after birth as well as later, during the hospital stay, even if they require intensive care.
Vitamin K should be applied immediately after the first postnatal hour during which skin-to-skin contact and the onset of breastfeeding should have occurred, to prevent its deficiency in newborns -which may expose them to bleeding.
The first dose of the hepatitis B vaccine should be administered to all newborns during their first 24 hours of life, as soon as possible after delivery. The vaccination schedule is completed with two more doses during the first year of life. It is estimated that more than 296 million people are infected with the hepatitis B virus, of which approximately 360 million are chronically affected and at risk for severe illness and death.
The hepatitis B virus vaccine is safe, effective, and provides over 95% protection.
Vitamin K and the hepatitis B vaccine should be administered as soon as possible during the first hours of life. They prevent complications such as bleeding derived from vitamin K deficiency and from the hepatitis B virus, which affects over 296 million people.
Timing of discharge of babies and their families from the Health Centre is a key piece of information regarding proper baby management at home.
This information includes post-bath drying techniques, skin-to-skin contact, eye care, thermal protection, exclusive breastfeeding, proper posture, nutrition, vaccination, administration of medications or multivitamins. It also provides details of warning signs, initial cardiopulmonary resuscitation manoeuvres in case of unexpected events and where to go in an emergency.
Parents should be briefed on the harm caused by tobacco and respiratory diseases including COVID 19.
Follow-up visits shall be coordinated in order to contribute to improve general care.
Discharge is the key piece of information regarding proper baby management at home. This information includes post-bath drying techniques, skin-to-skin contact, eye care, thermal protection, exclusive breastfeeding, proper posture, nutrition and vaccination. Future appointments shall be scheduled to contribute to improve general care.
Improper handling of oxygen may cause retinopathy of the prematurity (ROP) and other damage to immature neonates; to reduce the risks of harm, oxygen therapy safety limits must be strictly monitored.
The Basic Newborn Resuscitation Guidelines and the ROP Prevention Guidelines are very reliable support resources, with clear and consistent information for the implementation of safe measures. These guidelines clearly stipulate the limits for the administration and monitoring of the use of oxygen, in addition to establishing the appropriate levels to reduce the occurrence of ROP. Abiding by these guidelines diminishes the disease burden of ROP and improves the survival of premature newborns.
As inadequate handling of oxygen can cause damage to immature newborns, the use of oxygen must be monitored following Evidence-based Guidelines.
Preterm newborns have the right to be cared for in a stable environment involving both their families and the health care team. These emotionally supportive and responsive interactions favour early learning.
Families have the right to always be present and actively engaged in the care of their babies, even if they are at risk at birth or need hospitalization. Closeness with newborns encourages loving and sensitive care in primary caregivers, which is key to achieving the maximum development potential of babies.
The families of premature newborns have the right to create a stable environment to take care of the baby, in conjunction with the health care team. The family’s closeness with the baby encourages affectionate and sensitive care that favours the newborn’s maximum development potential.
Rooming-in makes it easier for the mother to recognize signs that the baby is ready to be fed (wakefulness, rotation and mouth movements). At this key moment in the establishment of the attachment bond, remaining together enables the baby to cry less and the mother to rest more. Fathers or other family members may also be present, to accompany and collaborate with the mother in caring for the baby.
Exclusively breastfed newborns should only suck at the mother's breast. Unless indicated, they should not receive any other foods or fluids nor suck other items such as bottles or pacifiers.
The administration of other foods may decrease the baby's interest in breastfeeding. The bottle may interfere with the encouragement of suction. If the baby loses interest in breastfeeding when satisfied or if it has difficulties in sucking, the demand for breastfeeding may decrease and generate less stimuli in the mammary gland thus leading to less milk production.
Rooming-in contributes to strengthen breastfeeding and bonding.
Contact with the health team for care following discharge is essential to assess the baby’s growth and development, identify risk situations and provide guidance.
If the delivery is in a health centre, the mother and newborn should receive postnatal care during at least the first 24 hours prior to discharge. In case of home-birth, the first postnatal contact should be as soon as possible, within 24 hours following birth.
At least three additional postnatal contact occasions with the health team are recommended for all mothers and newborns: on day 3 (48 to 72 hours postpartum), between days 7 to 14, and 6 weeks following birth.
The place for postnatal care contact is flexible, at home or at the health centre, and may be supplemented with additional contact by mobile phone.
Contact with the health team for care following discharge is essential to assess the newborn’s growth and development, identify risk situations and provide guidance to families. At least three outpatient visits are recommended between birth and six weeks of age.
Delayed rather than immediate umbilical cord clamping is beneficial for premature babies because it helps ensure a greater iron store, which may protect them in several aspects that improve their neurodevelopmental prognosis by:
A. Preventing anaemia, which has an impact on cognitive, motor and behavioural development.
B. Reducing the risk of intraventricular haemorrhage, necrotising enterocolitis and late-onset sepsis.
C. Decreasing the requirements for surfactant, mechanical ventilation and blood transfusions.
D. Increasing the levels of cerebral oxygenation and blood pressure.
Delaying the umbilical cord clamping from 30 to 60 seconds in premature newborns favours placental transfusion both in vaginal deliveries and in caesarean sections.
Timely umbilical cord clamping in preterm infants is beneficial both immediately and in the long term. Hence, it is recommended to delay the clamping of the umbilical cord between 30 and 60 seconds after birth.
All newborns, including premature infants, should be fed colostrum and human milk as early as possible after birth. The administration of colostrum or human milk in amounts that have no nutritional consequence is known as Trophic Enteral Feeding. This diet should be maintained for several days until full feeding is possible.
Like human milk, colostrum contains cells and factors that provide protection against a wide variety of infections, especially those occurring in the hospital. Colostrum is particularly rich in these anti-infective factors, and its ingestion during the first hour of life helps prevent neonatal mortality. In addition, it contains nutrients that enhance digestion and absorption, stimulate the maturation of the gastrointestinal tract, and promote neurodevelopment. This diet favours the establishment of the healthiest bacterial flora or microbiota in the human species, which will have an impact on many health aspects in adult life.
The initiation of feeding of premature babies with colostrum and human milk should begin as early as possible. One of their many benefits is that they contain cells and factors that provide protection against a wide variety of infections.
Perinatal and newborn care must be conducted by qualified professionals sensitive to the fact that pregnancy, delivery and the days following delivery are periods of great vulnerability. They also represent a window of opportunity to enhance the health of both women and babies throughout their lifetime.
Institutions must include in their vision and mission the desired profile of professionals to be incorporated into healthcare activity together with their level of training and anticipate room for continuous professional education plans.
Both access to services and profitability may be significantly improved through rational management of the distribution of the tasks and responsibilities of the health professionals. The state must ensure that institutions providing delivery and newborn care count with the necessary specialized human resources according to the type and level of care and develop training policies.
The period from gestation to postpartum is a time of vulnerability and represents a window of opportunity for health improvement that extends throughout the life course. The training of qualified human
Some severe health problems present a window of opportunity for treatment - occasionally definitive - when diagnosed early on. Follow-up programs allow their identification together with the possibility of addressing any potential harm and systematic monitoring. /p>
Early detection enabling a therapeutic approach improves quality of life. Health institutions that monitor pregnancies and provide newborn care must organise follow-up programs for the required specialties according to their level of complexity and user population.
In turn, follow-up programs require policies that ensure the necessary resources for the diagnosis and treatment of severe health problems or situations that may need additional care.
Health institutions that provide care during pregnancy and delivery must organise follow-up programs for the early detection of serious health problems. These programs need policies that ensure the necessary resources for the required care.
Postnatal care must also include a timely and efficient referral mechanism.
When delivery occurs in an institution, mothers and newborns should receive immediate care during at least the first 24 hours following delivery.
Health system management must consider that in the case of home-deliveries the first postnatal contact with qualified professionals should occur as soon as possible, always within the first 24 postnatal hours.
Deliveries in health institutions require the provision of postnatal care during at least the first 24 hours. In the case of home-deliveries contact with qualified professionals must occur within the first 24 hours.
Health professional training is not always sufficient to provide correct obstetric and neonatal care. The number of staff members must also be appropriate to meet quality and safety standards. Their distribution will vary according to the level of complexity of the institution, whether the care provided is for high- or low-risk pregnant women.
Health-care institutions are responsible for management while the effective provision of human resources is a state responsibility.
In addition to training an appropriate number of health professionals, human resource management in agreement with quality and safety standards is vital in obstetric and neonatal care.
Pregnancy supervision, the preparation for the delivery and the following days constitute sensitive moments for the reception of messages to prevent risk situations. It is also the right time to administer vaccines. Institutions must guarantee the provision of information and the application of vaccines in efficient care processes with qualified personnel.
In order to fulfil its role in risk- and disease-prevention, the state must incorporate issues such as the importance of vaccines and their access, as well as information on other prevention services provided by health institutions in its campaigns.
Pregnancy and postpartum favour a better reception of disease prevention messages and coincide with the vaccination period. Health institutions must ensure efficient vaccination processes supported by official information campaigns.
Congenital abnormalities are one of the main causes of death. It is therefore important that health institutions prioritize their prenatal diagnoses in order to provide the best opportunities to newborns. Scheduling the reception of the birth, and its eventual referral to a specialized treatment centre may determine the prognosis in many cases. Regionalization favours the timely referral of sick newborns due to congenital abnormalities. Initial newborn assessment is of vital importance for their early treatment since certain abnormalities are not always detectable before birth.
National programs should consider the prevention of congenital abnormalities whenever possible together with their surveillance, monitoring and impact on public health. Detection and referral must be inclusive and provide therapeutic opportunities, support and continuous care to all boys and girls alike, as well as to their families.
Prenatal diagnosis of congenital abnormalities offers more opportunities for treatment. Newborn screening impacts on prognosis. It is therefore crucial to include prevention, surveillance, and monitoring of these diseases within national health programs.
Screening programs identify disorders in newborns before they present symptoms and thus enable specific treatment. This may contribute substantially to reduce the burden of mortality and morbidity due to early conditions with long-term consequences.
Institutions that attend births and provide newborn care are responsible for the organization and effective execution of screening programs.
Every country has specific legislation that stipulates the spectrum of tests included in the screening. Health policies must facilitate access to the necessary items, devices and qualified staff for its implementation together with treatment and follow-up for the detected disorders.
Screening programs identify disorders in newborns before they present symptoms and thus enable their specific treatment. Every country has specific legislation stipulating the tests included and must be supported by health policies.