PAHO’s capacity to forge multicountry partnerships, resolve cross-border challenges and generate real-time analysis underpins its sustained success in managing the regional response to COVID‑19. Capturing and institutionalizing lessons learned is the next step.
2022 has been a year of reflecting, rethinking, and reshaping. Not only for our COVID‑19 pandemic response, but also for our understanding of what the pandemic’s lessons mean for the future of public health. The advantage we have at this stage of the pandemic is information. Thanks to our teams of technical experts, and their continuous analysis throughout wave after wave of infections, we now understand – at least in part – many of COVID‑19’s far-reaching effects, and we have some insight into the underlying factors that affect the success or failure of our mitigation efforts. We have used this knowledge in all our response activities.
The first year of the pandemic saw our all-consuming priorities focus on slowing transmission, managing cases, and preventing deaths. In 2021, thanks to huge donor support for the regional vaccination drive, we had the opportunity to help Member States make solid progress toward global coverage targets and establish innovative mechanisms for resolving distribution bottlenecks, tackling infrastructure challenges, and delivering on urgent implementation goals in record time.
“Despite the innumerable devastating consequences of the COVID-19 pandemic, we are proud of the legacy of enduring relationships created in times of need.”
However, as 2022 got underway, the quick-wins that propelled our initial vaccination roll out were overtaken by more complicated implementation challenges. We turned to research and analysis to better understand the heterogeneity in responses in the Region. Here, PAHO’s unique capacity to forge multicountry partnerships, convene regional players, and to collect data directly from countries, enabled us to identify barriers hindering vaccine uptake, resolve cross-border supply chain and procurement challenges, and isolate possible causes of poor outcomes. This flexibility has enabled us to maintain the momentum of our successful COVID‑19 response into its third full year and lay the foundation for the Region’s post-pandemic recovery.
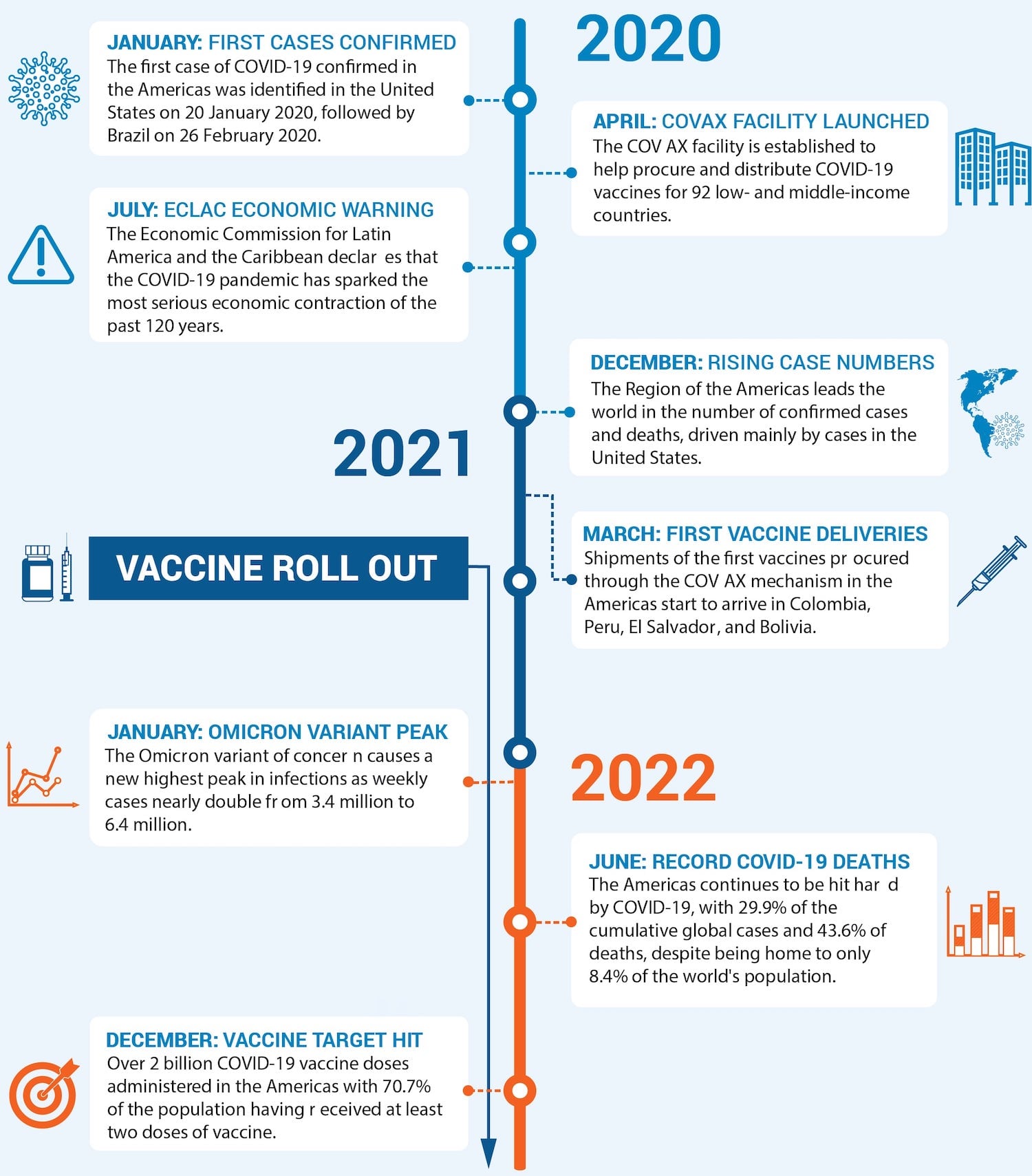
COVID-19 Response Timeline, 2020-2022
Current Vulnerabilities, Future Risks
More broadly, 2022 was the year when we began to reflect on the shift in global public-health thinking that emerged from the past three years of turmoil. The question of what this change of perspective might mean for the Region’s health challenges, and our support to countries as they advance in their pandemic recoveries, is now an urgent concern.
The staggering speed of the global spread of COVID‑19 forced us to reframe our vision of public health through a global health security lens. This viewpoint brought into stark relief the accumulative effect of vulnerabilities that characterize this region: economic inequalities, poverty and inequities, social exclusion, gender discrimination, and enormous disparities in health access and outcomes. These structural aspects combine with demographic and epidemiological transitions, as populations in many countries are aging, contributing to the already rising burden of noncommunicable diseases, and adding to the challenges of reemerging and new infectious diseases. Coupled with the unpredictable effects of climate change, these features become additive factors that constrain each country’s capacity to protect its people and shield neighboring states. COVID‑19 has shown us that each poorly managed health or social crisis is a clear impediment to responding to new health threats.
With full understanding of the enormity of this shift in thinking, PAHO has prioritized the identification, capture, and documentation of COVID‑19’s lessons for public health, including COVID-linked innovations that could help address longstanding health-sector challenges in other areas. In our flagship report, Health in the Americas, the summary of which was released in late 2022, we presented a thorough and wide-ranging examination of the COVID‑19 pandemic’s impact in the Americas and how it has reshaped our ideas.
“COVID‑19 has shown us that each poorly managed health or social crisis is a clear impediment to responding to new health threats.”
There were several significant findings:
COVID‑19 revealed the weakness of our prior efforts to predict which countries would perform well and those that would fare poorly. Comparing data from COVID‑19 mortality rates across the region with health system preparedness ratings, using methodology developed by the World Health Organization (WHO), demonstrated the lack of correlation between measures of preparedness and actual performance (mortality rates) during the pandemic. This observation was an important wake-up call about our understanding of the factors that determine a country’s response capacity.
The pandemic context provided an important opportunity to collect data that confirmed the role of social determinants of health, both as drivers of disease and disruptors of interventions that rely on personal decision-making. Modeling of mortality/morbidity risks combined with information about the difficulties experienced by those in vulnerable community settings with adhering to guidelines about social distancing or other prevention strategies, provides valuable insights. In particular, we gained new knowledge about barriers to health service access, disparities in outcomes, and the likely effectiveness of interventions for other conditions, such as many noncommunicable diseases, where community-based management or lifestyle interventions are key.
There can be little doubt that the pandemic spurred a significant advance of the digital transformation across the Region, in multiple sectors in multiple ways. We have data to show that this transformation is already having a positive impact on health care access and delivery, even in traditionally non-technologically literate communities such as the elderly. This culture shift promises even greater benefits in the future as health systems incorporate digital solutions into consultations, workflows, procurement processes, reporting, and recordkeeping.
The targeted negotiation and coordination work that was necessary to successfully procure, deliver, and assure the quality of millions of units of testing kits and reagents, vaccine doses, syringes, personal protective equipment, oxygen concentrators, and many other commodities for the Region is a real success story. We showed that using PAHO’s convening power to respond to country requests to facilitate inter-country cooperation was a key element in improving access to health technologies and addressing economic divides. We are excited about the potential of these new mechanisms for tackling other health challenges as we move forward.

During 2022, PAHO supported many countries in the Region to increase vaccination coverage among vulnerable groups. This image shows a vaccination fair held in Atlántida, Honduras, which promoted COVID-19 vaccination among Garifuna populations who are of mixed Afro-Caribbean and indigenous American descent.
Post‐COVID‐19 Primary Health Care
Finally, but perhaps most conceptually significant, COVID‑19 laid bare the weaknesses of a traditional primary health care-focused strategy in situations where emergency responsiveness is required. Our definition of primary health care, as enshrined in the Alma Ata Declaration of 1978, has been the cornerstone of global efforts to achieve universal access to health care and the attainment of the goal of Health for All for close to 50 years. However, the information we now have as a result of the COVID‑19 pandemic suggests that this definition may be insufficient to meet the demands of current and future health challenges. With aging populations and increasing burdens of chronic disease, our health systems must be equipped not only to offer traditional primary health care, but also to be emergency-ready, responsive, and able to provide effective acute care to address the needs of people with chronic conditions – who are both the most likely to present with emergency complications from their existing disease, and the most vulnerable to severe effects of new infectious threats. Public health in the post-COVID age is fundamentally changed, and we must adapt our basic assumptions to reflect this shift.
“Public health in the post‐COVID age is fundamentally changed. And we must adapt our basic assumptions to reflect this shift.”
PAHO’s Advantage: the Multiplier Effect
In presenting this summary report of our 2022 COVID‑19 response, supported by the generous contribution of US$ 75 million from the US Government, we are proud to show that money invested in PAHO’s activities in the Region generates long-lasting benefits that go far beyond the initial direct results. Careful layering of our interventions, while keeping vaccination coverage as our primary focus, has ensured that our investments have a multiplier effect.

PAHO’s 2022 COVID-19 response activities involved boosting COVID‑19 vaccine manufacturing capacity at the Institute of Technology in Immunobiologicals of the Oswaldo Cruz Foundation (Bio-Manguinhos/Fiocruz), Rio de Janeiro, Brazil, and across the Region.
With every activity implemented, information generated is used to refine and strengthen our work. The data we collect feed back into our analytical studies to develop practical guidance that informs decision-making at country level, and guides health professionals to deal with the crisis before them. Through our role on the global stage, as the regional arm of WHO, our hard-won knowledge shapes international norms and standard-setting work. No other health sector actor in the Region has the ability to harness this multi-channel, bidirectional information flow in the continuous process of reacting, responding, and rebuilding. And no other health sector organization has the depth and breadth of reciprocal relationships with Member States that ensure the power to implement, support, and sustain countries to drive change.
Despite the innumerable devastating consequences of the COVID‑19 pandemic, we are proud of the legacy of enduring relationships created in times of need, and strong partnerships and coordination systems that we know countries can count on for the future. The US Government’s substantial contribution to funding PAHO’s work means the entire Region benefits from our interventions. Our task now is to capture the substance of the innovations that have underpinned our practical successes and use them in our collective efforts to support countries to create the strong and resilient health systems the Region needs for the future.



