2.1 An overview of mortality and disease burden from noncommunicable diseases and external causes
Deaths and disease burden from noncommunicable diseases and external causes (2000–2019)
Chapter 1 explored life expectancy and mortality in the Americas, comparing three major causes of death (CMPN conditions, NCDs, deaths from external causes) between WHO regions 3 and PAHO subregions. 4 By 2019, 90% of all deaths and 89% of all disability-adjusted life years (DALYs) in the Americas were a result of NCDs and external causes, and much of the burden from lost life and lost health due to these causes is amenable to prevention and treatment.
Chapter 2 presents additional detail on the main contributors to NCDs and external causes. The chapter focuses on six broad causes of death and disability: cardiovascular diseases, cancers, respiratory diseases, diabetes, mental health and neurological conditions, and external causes (also known as injuries from unintentional and intentional causes). After a general introduction to these leading causes of death and disability, the chapter focuses on each of these six groups in turn. Section 2.2 describes the leading cardiovascular diseases, section 2.3 describes the leading cancers, section 2.4 describes the respiratory diseases, section 2.5 describes diabetes, section 2.6 describes the mental and substance use disorders and neurological conditions, and section 2.7 describes unintentional and intentional injuries.
The change in the numbers of deaths and DALYs between 2000 and 2019 is presented in Figure 10 by grouped causes of death and disability, for women and men separately. The numbers of deaths in all groups increased in the 20 years from 2000. From the smallest to largest change, the percentage increase in deaths for cardiovascular diseases was 15%, for deaths from external causes it was 24%, for cancers 31%, for respiratory diseases 40%, for diabetes 59%, and for mental and substance use disorders and neurological conditions, 179%. For the entire 20-year period, deaths in the Americas have been dominated by cardiovascular diseases and cancers, which in 2019 collectively accounted for 47% of all regional deaths.
Figure 10: The number of deaths and disability-adjusted life years (DALYs) in the Americas from noncommunicable diseases or external causes between 2000 and 2019 among women and men separately
The numbers of DALYs – the years of healthy life lost – also increased in all disease groups, with the largest percentage increases again for mental and substance use disorders and neurological conditions (a 47% increase) and for diabetes (an 88% increase). So, the relative importance of diabetes and of mental health and substance use disorders and neurological conditions as regional causes of lost life and lost health increased in the Americas between 2000 and 2019.
Certain gender differences are striking, with men in 2019 experiencing substantially more death and disability due to external causes, and substantially more disability due to cardiovascular diseases
Certain gender differences are striking, with men in 2019 experiencing substantially more death and disability due to external causes, and substantially more disability due to cardiovascular diseases. Each of these causes of death and disability groups are explored in more detail in sections 2.2 to 2.7.
Twenty leading causes of death and disability from noncommunicable diseases and external causes (2000 and 2019)
The 20 leading causes of death and disability from NCDs or external causes 5 in the Americas in 2000 and 2019 are presented in Figure 11 for women and men combined, using the age-standardized mortality and DALY rates per 100 000 people. (See also Box 2.)
Top 20 causes of death
Ischemic heart disease (IHD), strokes, and chronic obstructive pulmonary disease (COPD) have dominated regional deaths for the 20-year period since 2000. IHD (mortality rate of 73.6 per 100 000 in 2019) dominated the top three causes, with a rate that was 2.3 times higher than stroke (32.3 per 100 000) and 2.9 times larger than COPD (25.1 per 100 000). Alzheimer disease and dementias (mortality rate 22.3 per 100 000) and diabetes6 (20.9 per 100 000) made up the top five causes of regional deaths.
There have been important shifts in the relative importance of causes of death between 2000 and 2019. In particular, dementias rose from 11th to 4th most important cause of death (mortality rate increased from 11.8 to 22.3 per 100 000), drug use disorders rose from 27th to 14th (mortality rate increased from 2.7 to 8.0 per 100 000), and falls rose from 24th to 18th (mortality rate increased from 3.6 to 5.4 per 100 000).
Cancers were treated as 23 separate groups of conditions in this regional ranking, and they collectively dominated the causes of death, with 8 cancer groups in the top 20 causes in 2019, and with the top 5 cancers being trachea, bronchus, and lung cancers (7th position, mortality rate in 2019 of 18.7 per 100 000), breast cancer (8th position, 15.5 per 100 000 women), prostate cancer (9th position, 15.2 per 100 000 men), colorectal cancer (12th position, 9.8 per 100 000), and cervical cancer (15th position, 6.1 per 100 000 women).
Figure 11: The 20 leading causes of death (using mortality rate per 100 000) and disability (using disability-adjusted life years [DALY] rate per 100 000) in 2000 and in 2019 in the Americas
Note: These are leading causes from the six broad causes of death and disability: cardiovascular diseases, cancers, respiratory diseases, diabetes, mental health and neurological conditions, and external causes.
Data source:World Health Organization. Mortality and global health estimates.
BOX 2: The 20 leading causes of death (using number of deaths) and disability (using number of disability-adjusted life years [DALYs]) in 2019 in the Americas, all causes
Analysts use different methods to rank the relative importance of different causes. Figure 11 uses age-standardized rates (mortality rates to rank importance as a cause of death, DALY rates to rank importance as a cause of disability). Because of the focus of this report (noncommunicable diseases [NCDs], mental and substance use disorders and neurological conditions, and injuries), only these causes have been used in the ranking in Figure 11. For causes always or mostly occurring in women or men (breast cancer, prostate cancer, cervical cancer) sex-specific rates have been used (female rates for breast and cervical cancer, male rates for prostate cancer). Another way to explore the relative importance of causes is to use the absolute number of deaths or DALYs, and to consider all causes, including for example the communicable, maternal, perinatal, and nutritional (CMPN) conditions. Using this method, the 2019 ranking for deaths and disease burden is shown below. The five colors (red to blue) represent quintiles of each top-20 ranking. Causes in the top-20 deaths or the top-20 disease burden, but not both, are shown with a dark center. In this alternative presentation, the sex-specific cancers have lower mortality ranking and do not feature in the disease burden rank. Some conditions not covered by this report but in the ranking include lower respiratory infections, kidney diseases, liver cirrhosis, and neonatal conditions.
Top 20 causes of disease burden
Disease burden, measured using the DALY rate, was also dominated by IHD, with a rate of 1515 lost years of health per 100 000 in 2019, down from 2291 per 100 000 in 2000. Some illnesses did not feature as a cause of death but were important causes of disease burden, notably depressive disorders (7th most important cause of disease burden, DALY rate in 2019 of 658 per 100 000), anxiety disorders (9th position, DALY rate 534 per 100 000), alcohol use disorders (14th position, 388 per 100 000), and migraines (15th position, 379 per 100 000). Other illnesses did feature in the top 20 causes of death, and were even more important as causes of lost health, notably interpersonal violence (6th most important cause of death, 2nd most important cause of lost health), road injuries (10th position, 4th position), drug use disorders (14th position, 6th position), and falls (18th position, 13th position). Five illnesses gained importance as causes of lost health in the 20 years since 2000: Alzheimer disease and dementias (rising from 20th to 16th most important cause of lost health), self-harm (16th to 11th), drug use disorders (12th to 6th), diabetes (5th to 3rd), and interpersonal violence (3rd to 2nd).
Unconditional probability of dying between 30 and 70 years of age (2015 and 2019)
The Sustainable Development Goal (SDG) target 3.4 is to reduce premature mortality from NCDs by a third by 2030 relative to 2015 levels, and to promote mental health and well-being. Premature mortality for this target is defined as mortality between 30 and 70 years of age, and NCDs include four of the six grouped causes considered in this report: CVD, cancers, respiratory diseases, and diabetes. Progress toward target 3.4 is being monitored by a consortium including WHO (3). Progress in the Americas by 2019 is summarized in Figure 12.
The baseline probability of dying between 30 and 70 years of age (30q70) in 2015 ranged from 3.1% in the Andean subregion to 5.9% in the Latin Caribbean (Figure 12, right-hand panel). By 2019, this probability had fallen in all subregions, with reductions above 6% in the Southern Cone and Andean subregions, reductions between 4% and 6% in Brazil, Central America, and Latin Caribbean, reductions between 2% and 4% in North America and non-Latin Caribbean, and a reduction of less than 1% in Mexico. In the four years from 2015, these reductions translate to annual percentage reductions of between 0.13% in Mexico and 1.72% in the Southern Cone subregion. An annual reduction over 2% will eventually be required to achieve a 33% reduction in NCD premature mortality over 15 years.
2.2 Cardiovascular diseases
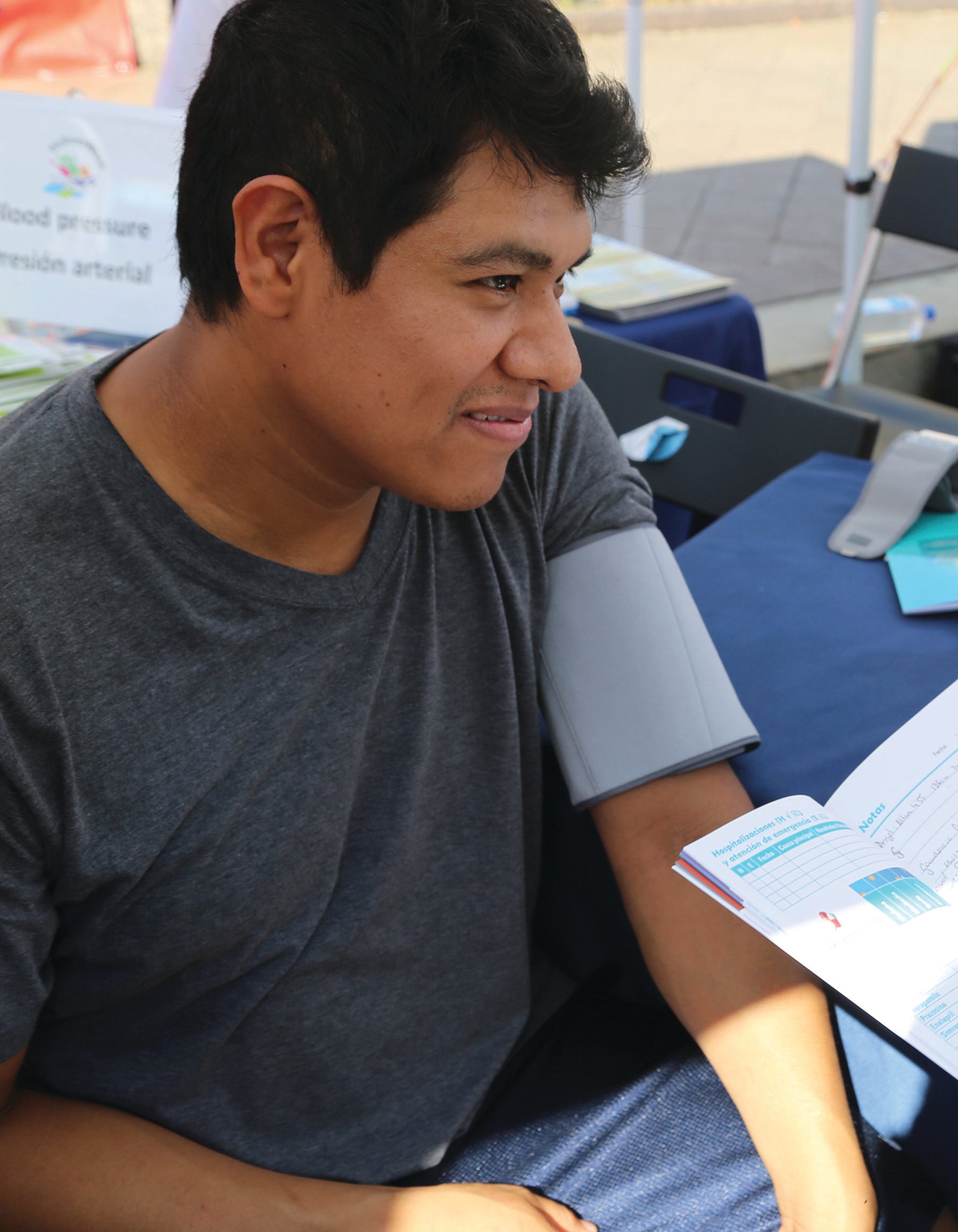
Cardiovascular diseases (CVD) is a general term for conditions affecting the heart or blood vessels. The risk of certain CVDs may be increased by high blood pressure or cholesterol, smoking, unhealthy diet, lack of exercise, obesity, excessive alcohol consumption, or poor sleep. Diabetes, itself a major cause of disability and death, is also a recognized CVD risk factor. These risk factors have been reliably linked to lifestyle, which in turn is influenced by a person's social circumstances. Because of the association of CVD with lifestyle, a large proportion of CVD deaths are assumed to be preventable or delayable through interventions, for example, to promote healthy eating, to help avoid tobacco smoke, and to limit alcohol intake. Cost-effective treatments to lower blood pressure and lipids or to control diabetes are also widely implemented.
Leading causes of death and disease burden
The absolute number of CVD deaths in the Americas increased from 1.76 million in 2000 to 2.02 million in 2019. Total deaths in the Region also increased, from 5.46 million in 2000 to 7.16 million in 2019, so that the share of deaths due to CVD decreased slightly, from 32.3% in 2000 to 28.3% in 2019. The five leading causes of CVD deaths in the Americas in 2019 are summarized in Table 4.
General cardiovascular disease trends
For four of the five leading causes of CVD (hypertensive heart disease is the exception), there have been important reductions in death and DALY rates. For women and men combined, the reductions have ranged from 35% to 45% for death rates, and from 31% to 34% for DALY rates. These death and DALY rate improvements are a critical and welcomed step on the pathway to improved population health, and point to the importance of healthcare interventions across the Region. The rate reductions, however, were not large enough to offset the region's increasing population, and its rapid aging, so that overall the number of CVD deaths and years of life lost have continued to increase. There have been exceptions, with the number of IHD deaths decreasing slightly among women; cardiomyopathy, myocarditis, and endocarditis deaths and DALYs decreasing slightly among women; and rheumatic heart disease deaths and DALYs decreasing among women and men.
The region's population size has been discussed in Chapter 1 (section 1.2, Table 2), and the health challenges associated with population growth and population aging are discussed in Chapter 3.
Notes: a Mortality is described using the age-standardized mortality rate. Disease burden is described using the age-standardized DALY rate. Both rates presented per 100 000 population. b Ischemic heart disease. c Hypertensive heart disease. d Cardiomyopathy, myocarditis, endocarditis. e Rheumatic heart disease. f All CVD includes “other” circulatory diseases (All CVD ICD-10 codes: I00–I99. Other CVD ICD-10 codes: I00, I26–I28, I34–I37, I44–I51, I70–I99).
Data source:World Health Organization. Mortality and global health estimates.
Again, for four of the five leading causes of CVD (rheumatic heart disease is now the exception), men were disproportionately affected, with a higher burden of deaths and DALYs. In 2019 the ratio of male to female death rates ranged from 1.18 to 1.80, and the range for DALY rates was 1.14 to 2.03. There were 1.04 million deaths and 23.0 million years of lost health in 2019 among men, compared to 981 000 and 17.9 million among women.
Ischemic heart disease since 2000
Coronary artery disease (narrow or blocked coronary arteries) can lead to ischemic heart disease (IHD), which in 2019 accounted for 15% of all deaths, and over half (54%) of all CVD deaths in the Americas. The IHD mortality rate has improved considerably since 2000, down by 37% to 74 IHD deaths per 100 000 people. This 20-year improvement has been similar in women and men, with the mortality rate among men improving from 149 in 2000 to 96 in 2019 (a 36% improvement), and the rate in women improving from 92 in 2000 to 55 in 2019 (a 41% improvement). Nonetheless, many more men continue to die from IHD, with the mortality rate ratio rising gently from 1.61 in 2000 to 1.75 in 2019, and over 600 000 men dying of IHD in 2019, 110 000 more deaths than among women. Similar improvements were seen in the IHD DALY rate, with the rate among men down from 3074 per 100 000 people in 2000 to 2071 per 100 000 in 2019 (a 33% improvement), and the rate among women down from 1614 per 100 000 in 2000 to 1021 per 100 000 in 2019 (a 37% improvement). So, in 2019 the DALY rate among men remained at twice the level for women (DALY rate ratio 2.03). There were 12.3 million years of lost health among men in 2019, compared to 7.7 million lost years among women.
Stroke since 2000
A stroke is a serious and often life-threatening condition that happens when the blood supply is cut off to part of the brain. An ischemic stroke is more common and is caused by a blood clot. A hemorrhagic stroke occurs when a weakened blood vessel supplying the brain bursts. Rapid diagnosis and treatment is crucial to limit the damage. After IHD, stroke is the second most common cause of CVD death and disability. In 2019, the regional stroke burden was roughly half that of IHD, with 478 000 deaths and 10.3 million years of lost health. Like IHD, rates have improved consistently since 2000, with the death rate down from 49.9 to 32.3 per 100 000 (a drop of 35%) and the DALY rate down from 1172 to 797 per 100 000 (a drop of 32%). The gender difference again favored women but was less pronounced than for IHD (mortality rate ratio 1.18, DALY rate ratio 1.14). Although rates of stroke were a little lower among women, the larger number of women alive in the older age groups mean that more women died from stroke in 2019 (257 000 deaths among women, 220 000 deaths among men), and there were more years of lost health among women (5.31 million years among women, 5.02 million years among men).
Hypertensive heart disease since 2000
Over time, untreated hypertension can lead to a thickening of the heart wall, and this is an important step in the pathway toward heart failure and other less common outcomes, collectively known as hypertensive heart disease (HHD). Hypertensive heart disease is the only major CVD with mortality rates and DALY rates that have increased in the past 20 years. Deaths increased from 81 000 in 2000 to 157 000 in 2019, and mortality rates in women and men combined from 9.5 per 100 000 to 10.6 per 100 000 (a 12% increase). Similarly, years of healthy life lost increased from 1.70 million in 2000 to 3.02 million in 2019, with a DALY rate increase of 212 to 232 per 100 000 (a 9% increase).
Cardiomyopathy, myocarditis, and endocarditis since 2000
A group of conditions affecting the heart muscle, including stretching, thickening, or stiffening of the heart chambers that is mostly inherited (cardiomyopathy), inflammation of the heart muscle often caused by a viral infection (myocarditis), or inflammation of the inner lining of the heart's chambers and valves often caused by a bacterial infection (endocarditis).
The burden from this group of conditions is less than one-tenth that of IHD, and there have been similar 20-year reductions in burden since 2000. The mortality rate for women and men combined dropped from 7.9 to 5.1 per 100 000 (a 36% decrease), and the DALY rate dropped from 232 to 155 per 100 000 (a 33% decrease). Men were again disproportionately affected (mortality gender rate ratio 1.80 in 2019); there were 39 000 deaths and 1.1 million DALYs among men in 2019, compared to 29 000 deaths and 680 000 DALYs among women.
Rheumatic heart disease since 2000
Rheumatic heart disease is a condition in which the heart valves have been permanently damaged by rheumatic fever. Rheumatic fever is a disease of poverty and has been mostly eliminated in high-income countries. Although still problematic in the Americas, the mortality rate dropped from 1.3 to 0.7 per 100 000 (a fall of 45%) and almost two-thirds of all deaths occurred in just two countries: Brazil (2192 deaths), where rheumatic fever remains endemic; and the United States (3645 deaths), where rheumatic fever is uncommon and cases of rheumatic heart disease are likely to be among immigrant communities.
Deaths across the life course
Figure 13 presents the proportion of deaths and DALYs in each of five age groups: under 5s, 5–19, 20–39, 40–64, 65+. For IHD, stroke, and HHD, just over three-quarters of all deaths were among adults aged 65+. Among the remaining two conditions – cardiomyopathy, myocarditis, and endocarditis, and rheumatic heart disease – around two-thirds of all deaths were among adults aged 65+, with the remaining one-third split between young adults (20–39 years) and adults aged 40–64 years. For IHD, stroke, and HHD the full disease burden measured by DALYs was roughly split between adults aged 40–64 (one-third of the entire burden) and adults aged 65+ (two-thirds). Among the remaining two conditions – cardiomyopathy, myocarditis, and endocarditis, and particularly rheumatic heart disease – the full disease burden was split more evenly across the age groups, with older children (aged 5–19) and all adults affected.
Regional inequalities
Regional and subregional averages can mask important inequalities between countries. Figure 14 presents 2019 mortality rates for each of the five leading causes of CVD. Each bar represents the mortality rate for one country, the bars are ordered from high to low mortality rates, and the black bar represents the mortality rate for the entire Region of the Americas. Countries with the highest five and lowest five mortality rates are listed on the chart. The index of disparity (IoD) is presented on the chart and is an overall measure of inequality between countries – the larger the value the higher the regional inequality for that cause of death.
Between-country inequalities in mortality rates were highest for rheumatic heart disease (IoD 90) and lowest for IHD (IoD 38). For rheumatic heart disease, this inequality was driven by Haiti with a mortality rate of 9.1 per 100 000. Most countries had a small number of estimated deaths due to rheumatic heart disease, so that 23 of the 33 countries had a mortality rate below 1 per 100 000. The higher regional mortality rate inequalities for stroke (IoD 86) and for HHD (IoD 79) were partly driven by higher Caribbean rates. The three highest stroke mortality rates in 2019 were seen in Haiti (163 per 100 000), in Guyana (149 per 100 000), and in Suriname (117 per 100 000), and 11 of the highest 15 rates were in the Caribbean. The 2019 stroke mortality rate in Haiti was 11 times greater than the lowest regional rate (Canada, 15.1 per 100 000) – compared to Canada, there were 148 additional stroke deaths in Haiti per 100 000 people. The situation was similar for HHD, with the highest three mortality rates in The Bahamas (53 per 100 000), in Guyana (46 per 100 000), and in Haiti (37 per 100 000), and with 10 of the highest 15 rates in Caribbean countries. The 2019 rate in The Bahamas was over 25 times greater than the lowest regional rate (El Salvador, 2.1 per 100 000) – compared to El Salvador, there were 51 additional HHD deaths in The Bahamas per 100 000.
2.3 Cancers
Cancer is a group of diseases in which some of the body's cells grow uncontrollably, eventually spreading to other parts of the body. This process of spreading is known as metastasis and is the main cause of cancer death. The change from normal cells to cancerous (tumor) cells results from an interaction between a person's genetic factors and external cancer-causing agents known as carcinogens. There are a very wide range of known or suspected risk factors for cancer. Tobacco use is strongly linked to an increased risk for many types of cancer, certain viruses and bacteria can cause cancer, and radiation is also a known cause. Aspects of our diet, including alcohol, physical activity, obesity, and many environmental chemicals and pollutants may also increase our risk of certain cancers. Reducing or eliminating exposure to carcinogens is key to any prevention strategy, and early detection, sometimes as part of a population screening program, can improve the outcomes among people living with cancer.
Leading causes of death and disease burden
The absolute number of cancer deaths in the Americas increased from 1.04 million in 2000 to 1.36 million in 2019. This 20-year increase broadly tracked the increase in total regional deaths, so that the percentage of regional deaths due to cancer remained static at around 19%. The 10 leading causes of cancer deaths in the Americas in 2019 are summarized in Table 5.
Notes: a Mortality is described using the age-standardized mortality rate. Disease burden is described using the age-standardized DALY rate. Both rates presented per 100 000 population. b Lung cancer also includes the relatively rare cancers of the windpipe (trachea) and the glands and ducts of the lung airways (bronchi). c Breast cancer is presented for women only. There were a small number of breast cancer deaths among men: 813 deaths in 2000, rising to 1050 deaths in 2019. d Colorectal cancer is known as colon cancer or rectal cancer depending on where it starts. e Cervical cancer is also known as cervix uteri cancer. f “All cancers” include “other” cancers (All cancers ICD-10 codes: C00–C97. Other cancers ICD-10 codes: C17, C26–C31, C37–C41, C46–C49, C51, C52, C57–C60, C63, C68, C69, C74–C75, C77–C79).
Data source:World Health Organization. Mortality and global health estimates.
General cancer trends
For 9 of the 10 leading causes of cancer deaths (liver cancer is the exception) mortality rates and rates of disability have dropped in the 20 years from 2000. Overall, the cancer mortality rate fell by 21% (down from 128 per 100 000 in 2000 to 101 per 100 000 in 2019). As with the cardiovascular diseases, these improvements reflect the important public health and healthcare initiatives ongoing across the region. The gains are large, but do not fully offset regional population growth and aging, so that the absolute numbers of cancer deaths and years living with cancer disability have increased since 2000.
Three of the 10 cancers are sex-specific (prostate cancer in men, cervical cancer in women, and breast cancer mostly in women). For the remaining seven cancers, men are disproportionately affected, with higher mortality rates and higher rates of disability. In 2019, the ratio of male to female death rates ranged from 1.27 to 1.79, and the range for DALY rates was 1.31 to 1.80. In 2019, there were 707 000 deaths and 16.7 million years of lost health among men, compared to 654 000 and 16.1 million among women.
Trachea, bronchus, and lung cancers since 2000
This group of cancers is dominated by lung cancer. Although people who have never smoked can develop lung cancer, smoking is the most common cause, accounting for around 70% of cases (4, 5). Lung cancer does not cause noticeable symptoms until it has spread through the lungs or to other parts of the body, and for this reason the outlook for people with lung cancer is not as good as for other cancers. Despite a consistent annual improvement in mortality rate, lung cancer has been the leading cause of cancer death and disability in the Americas since 2000.7 In 2019 lung cancer ccounted for 4% of all deaths in the Americas, and 19% of all cancer deaths. It caused 56 000 deaths and 5.5 million years of lost health. The 20-year improvement in lung cancer mortality rates has been greater in men than in women, with the mortality rate among men improving from 39 per 100 000 in 2000 to 23 per 100 000 in 2019 (a 40% improvement), and the rate in women improving from 20 per 100 000 in 2000 to 15 per 100 000 in 2019 (a 23% improvement). Although more men continue to die from lung cancer (143 000 men died of lung cancer in 2019, 30 000 more deaths than among women), the mortality gender rate ratio dropped from 2.0 in 2000 to 1.5 in 2019, highlighting a narrowing of this gender difference.
The 20-year improvement in lung cancer mortality rates has been greater in men than in women, with the mortality rate among men improving from 39 per 100 000 in 2000 to 23 per 100 000 in 2019
Breast cancer since 2000
In countries that collect data, breast cancer is regularly the most common cancer among women. In the United States, for example, about one in eight women will develop invasive breast cancer during their lifetime (6). When detected early there is a good chance of recovery, and campaigns to encourage regular breast examinations or screening are a feature of many countries. Although rare, breast cancer can also occur in men. Among women in 2019, breast cancer was the leading cause of cancer deaths (jointly with lung cancer) and was the leading cause of cancer disability in the Americas. In 2019, the breast cancer mortality rate was 16 deaths per 100 000 (lung cancer in women was 15 deaths per 100 000), and the DALY rate was 490 per 100 000 (lung cancer in women was 349 lost years of healthy life per 100 000). Breast cancer rates have improved consistently since 2000, with the mortality rate down from 19 per 100 000 (a drop of 19%) and DALY rate down from 597 per 100 000 (a drop of 18%).
Prostate cancer since 2000
In countries that collect data, prostate cancer is regularly the most common cancer among men. In the United States, for example, about one in eight men will develop prostate cancer during their lifetime (6). Prostate cancer mostly occurs in later life, generally in men over 50 years of age. It usually progresses slowly, so that a man with prostate cancer may live for decades without symptoms or needing treatment. Prostate cancer is the second most common cause of cancer deaths and disability among men in the Americas. In 2019, the prostate cancer mortality rate was 15 deaths per 100 000 (the lung cancer mortality rate in men was 23 deaths per 100 000), and the DALY rate was 296 per 100 000 (the lung cancer DALY rate in men was 512 lost years of healthy life per 100 000). Prostate cancer rates have improved consistently since 2000, with the mortality rate down from 21 per 100 000 (a drop of 26%) and DALY rate down from 384 per 100 000 (a drop of 23%).
Colon and rectum cancers since 2000
Colorectal cancer is also known as colon cancer or rectal cancer depending on where it starts. Most people with colorectal cancer are aged 60 years or older. Although specific causes are not known, the common lifestyle risk factors for NCDs (such as physical inactivity, obesity, alcohol consumption) are thought to play a part. A diet low in fiber and high in processed meat can increase risk, as can a family history of early onset colorectal cancer. Colorectal cancer in 2019 in the Americas caused 134 000 deaths (68 000 deaths among men, 65 000 among women), and 3.1 million years of lost healthy life (1.6 million years among men, 1.4 million among women). Mortality rates improved gently between 2000 and 2019, down from 15 to 11 deaths per 100 000 among men (a 23% improvement) and from 11 to 9 per 100 000 among women (a 21% improvement).
Cervical cancer since 2000
Cervical cancer originates in the cervix – the neck of the womb. Nearly all cervical cancers are caused by human papillomavirus (HPV), and for this reason cervical screening programs are a feature of cancer prevention in many countries. HPV vaccination is available across the region, making cervical cancer largely preventable. Although mortality rates have fallen by 24% since 2000, across the Americas almost 39 000 women died from cervical cancer in 2019, up from 33 000 twenty years ago. This increase partly reflects the growing population of the Americas and also points to the need for continued communication campaigns highlighting the importance of vaccination and screening. HPV vaccination coverage has a target of 90% of girls by age 15, but falls short of this in many countries (7).
Other top 10 cancers since 2000
Five more cancer sites make up the top 10 causes of cancer deaths in the Americas: pancreatic cancer, lymphomas and myelomas, stomach cancer, liver cancer, and leukemia. Mortality rates for these cancers in 2019 ranged from 4 to 6 per 100 000, and rates of disability ranged from around 123 to 153 years of lost health per 100 000. Mortality rates for three of the five cancers (the lymphomas and myelomas, stomach cancer, leukemia) have dropped noticeably since 2000, falling by between 20% and 30%. The mortality rate for pancreatic cancer has remained roughly unchanged, dropping by just 2% over 20 years, and liver cancer is the only condition to see a mortality rate increase, rising 11% since 2000.
Deaths across the life course
Cancers occur with increasing frequency as we age, most likely due to the accumulation of risk over time and the reduced ability of the aging body to effectively make cellular repairs. Figure 15 presents the proportion of deaths and DALYs in each of five age groups: under 5s, 5–19, 20–39, 40–64, 65+.
For most cancers, between half and three-quarters of all deaths occurred among adults aged 65+. Cervical cancer was the notable exception, with more adults aged 40–64 (49%) dying than adults aged 65+ (39%). Breast cancer also had a younger age profile at death, with adults aged 40–64 contributing 40% of all deaths. Only prostate cancer reported deaths almost exclusively among adults aged 65+. Years of healthy life lost was also dominated by the older age groups, but the percentages reflected a sizable proportion of adults aged 40–64 also living with cancer. For breast, cervical, stomach, and liver cancers, more years of healthy life were lost among adults aged 40–64 than aged 65+. Overall, the years of healthy life lost among all cancers was roughly the same for adults aged 40–64 (14.3 million, 44% of all healthy years lost) and adults aged 65+ (15.2 million, 46% of all healthy years lost). Leukemia stood apart, with all age groups contributing to the years of healthy life lost.
Regional inequalities
Among the 10 leading causes of cancer, the largest between-country differences in mortality rates were seen for cervical (IoD 100) and prostate cancers (IoD 105) (Figure 16). For both cancers, variation in the coverage of screening (and for cervical cancer vaccination) is likely to contribute to these higher inequalities. The United States and Canada, with high screening and vaccination coverage, have rates among the lowest five countries. Caribbean countries have noticeably higher mortality rates for breast and prostate cancer, contributing to mortality rate inequalities in these two cancers. For prostate cancer, all 13 Caribbean countries (along with Belize in Central America) have higher mortality rates than the rest of the Americas. For breast cancer, 12 of the highest 15 mortality rates are in Caribbean countries. These cancer disparities reflect relationships among many factors, including social circumstances, behavior, biology, and genetics – all of which can have profound effects on health, including cancer risk and outcomes. There is reliable evidence, for example, that women of African descent have a higher prevalence of triple-negative breast cancer, with poorer rates of survival (8).
2.4 Respiratory diseases
Respiratory diseases (RD) are conditions affecting the lungs and airways. The most common of these are chronic obstructive pulmonary disease (COPD) and asthma, but there are many others, including pulmonary hypertension (high blood pressure in the blood vessels that supply the lungs), and a range of occupational lung diseases. Tobacco smoke is the main RD risk factor, and there are many others including indoor and outdoor air pollution, and occupational chemicals and dust. RDs are not curable, and treatment focuses on expanding the airways to relieve symptoms and improve the quality of life of people living with RD. The WHO Global Alliance against RDs (GARD) aims to improve diagnosis and treatment of RD, focusing in particular on the needs of people with RDs in low-income and middle-income countries (9).
Leading causes of death and disease burden
The absolute number of RD deaths in the Americas increased from 382 000 in 2000 to 534 000 in 2019. This 20-year proportional increase was larger than the increase in total regional deaths, so that the percentage of all deaths due to RD increased slightly, from 7.0% in 2000 to 7.5% in 2019. The leading causes of RD deaths in the Americas in 2019 are summarized in Table 6.
Notes: a Mortality is described using the age-standardized mortality rate. Disease burden is described using the age-standardized DALY rate. Both rates are presented per 100 000 population. b Other RDs include a range of occupational lung diseases from inhaling chemicals or dust in the workplace. (All RDs ICD-10 codes: J30–J98. Other RDs ICD-10 codes: J30–J39, J47–J98.)
Data source:World Health Organization. Mortality and global health estimates.
Chronic obstructive pulmonary disease since 2000
COPD is the name for a group of lung conditions that cause breathing difficulties. It includes emphysema – damage to the air sacs in the lungs, and chronic bronchitis – long-term inflammation of the airways. COPD is common among older adults who smoke, so is largely preventable by avoiding smoking. Certain dusts and chemicals in the workplace have also been linked to COPD. At first, many people do not realize they have the condition, and it tends to get gradually worse over time, limiting normal activities. Treatment can help to control the symptoms of breathlessness, cough, wheezing, and chest infections. Common treatments include inhalers, medicines, and specialist exercises designed to make breathing easier. COPD accounted for 5% of all deaths, and almost three-quarters (71%) of all RD deaths in the Americas. The COPD mortality rate has improved since 2000, down by 18% to 25 COPD deaths per 100 000 people. This 20-year improvement has been much greater in men than women, with the mortality rate among men improving from 40 in 2000 to 30 in 2019 (a 27% improvement), and the rate in women improving from 24 in 2000 to 22 in 2019 (a 10% improvement). Although the COPD mortality rate remained higher among men, the region has more older women, so that for the first time, in 2019, the number of COPD deaths among women exceeded the number among men (189 122 deaths among men, 189 184 deaths among women). Similar improvements were seen in the COPD DALY rate, with the rate among men down from 929 per 100 000 people in 2000 to 710 per 100 000 in 2019 (a 24% improvement), and the rate among women down from 665 per 100 000 in 2000 to 585 per 100 000 in 2019 (a 12% improvement). There were 4.3 million years of lost health among men in 2019, compared to 4.4 million lost years among women.
Asthma since 2000
Asthma is a common lung condition that causes occasional breathing difficulties. Inflammation and narrowing of the small airways in the lungs cause asthma symptoms, which can be any combination of cough, wheeze, shortness of breath, and chest tightness. It affects people of all ages and often starts in childhood, although it can also develop for the first time in adults. There is currently no cure, but there are simple treatments that can help keep the symptoms under control, so it does not need to adversely affect quality of life. Asthma in 2019 caused 13 000 deaths (5000 deaths among males, 8000 deaths among females). Since 2000, asthma mortality rates have fallen from 1.9 per 100 000 to 1.0 per 100 000, an improvement of 47%. Unlike COPD, the improvement has been roughly the same in females and males. Although mortality from asthma is low and falling, it can cause many years of lost health. In 2019 it was responsible for 2.8 million years of lost health, up from 2.4 million in 2000. The DALY rate in 2019 was 280 per 100 000, almost unchanged over 20 years.
Deaths across the life course
Figure 17 presents the proportion of deaths and DALYs in each of five age groups: under 5s, 5–19, 20–39, 40–64, 65+. The age profile for COPD and asthma were fundamentally different. COPD, with its environmental causes and gradual onset, almost exclusively affected older adults. In contrast, the burden from asthma was spread across the life course.
Regional inequalities
In 2019, the country with the lowest COPD mortality rate in the region was Trinidad and Tobago (7 deaths per 100 000), which would see 18 fewer deaths per 100 000 people than the regional average for the Americas (25 per 100 000) and 42 fewer deaths per 100 000 than the country with the highest mortality rate (Honduras, 49 per 100 000)(Figure 18). The overall regional COPD inequality (IoD 34) was similar to that seen in IHD, for example (IoD 38). The overall regional mortality rate inequality for asthma was much higher (IoD 143) and this was driven by an extremely high mortality rate in Haiti (13 deaths per 100 000) compared to the next highest rate in Honduras (5 per 100 000) and a group of seven countries with mortality rates below 1 per 100 000 (Argentina, Canada, Chile, Colombia, Ecuador, Peru, United States).
2.5 Diabetes
We get our energy from the foods we eat, converting carbohydrates to sugar (glucose). Once glucose is in the bloodstream, insulin produced in the pancreas causes cells throughout the body to absorb the sugar and use it for energy. Diabetes occurs when the body does not use insulin properly or does not make enough insulin, leaving too much glucose in the blood. Abnormally high blood glucose levels can lead to acute problems, and if it persists over time can lead to serious, chronic complications that are difficult to reverse. A small fraction of patients with diabetes are unable to make insulin at all, and this is known as type 1 diabetes. For most people living with diabetes – as many as 95% – insulin is produced but is less effective at lowering blood sugar, and this is known as type 2 diabetes. People living with type 1 diabetes require daily insulin. People living with type 2 diabetes can use a combination of lifestyle change, medication, or insulin to control their blood sugar.
Leading causes of death and disease burden
Diabetes since 2000
The absolute number of diabetes8 deaths in the Americas increased from 178 000 in 2000 to 284 000 in 2019. This 20-year proportional increase was larger than the increase in total regional deaths, so that the percentage of all deaths due to diabetes increased, from 3.3% in 2000 to 4.0% in 2019. Diabetes as a cause of death and disability in the Americas in 2019 is summarized in Table 7.
Notes: a Mortality is described using the age-standardized mortality rate. Disease burden is described using the age-standardized DALY rate. Both rates are presented per 100 000 population. b Throughout this report, diabetes is defined as ICD-10 codes E10–E14 (minus E10.2, E11.2, E12.2, E13.2, E14.2). This classification includes insulin-dependent diabetes, non-insulin-dependent diabetes, and malnutrition-related diabetes. It does not include diabetes arising in pregnancy (gestational diabetes) or diabetes-related renal complications (these are included in a separate categorization of kidney diseases).
Data source:World Health Organization. Mortality and global health estimates.
The diabetes mortality rate has improved marginally since 2000, down by 5% to 21 deaths per 100 000 people. This 20-year improvement has been driven by an improvement among women. The rate in women improved from 22 per 100 000 in 2000 to 19 in 2019 (a 13% improvement), whereas the rate among men rose slightly from 22 in 2000 to 23 in 2019 (a 4% increase). The increasing prevalence of diabetes across the region (10) – linked partly to the falling mortality – has fueled a dramatic increase in the years of full health lost because of diabetes, up from 7.2 million years in 2000 to 13.4 million years in 2019. The diabetes DALY rate increased from 925 years per 100 000 in 2000 to 1082 years in 2019 (a rise of 17%), with a much larger rate rise in men compared to women (25% DALY rate rise among men, compared to a 10% rate rise among women).
In 2019 men had a higher diabetes mortality rate and DALY rate compared to women across the region (gender rate ratio 1.2 in both cases). These gender ratios have increased from parity in 2000. Looking at the DALY gender rate ratio since 2000 in the eight subregions of the Americas (Figure 19), the 2019 excess burden among men is currently driven by large and long-standing excesses in the North America and Southern Cone subregions. Perhaps more dramatically, the figure highlights a trend of worsening male outcomes, compared to women, in all subregions except Central America. Even the Latin Caribbean, where women in 2019 lost more years of healthy life due to diabetes than men (DALY rate in 2019, 0.83), the relative burden of male diabetes has been increasing. Gender differences in risk factor profiles and uptake of comprehensive care solutions for people living with diabetes are likely contributors to this switching diabetes burden.
Deaths across the life course
Figure 20 presents the proportion of deaths and DALYs in each of five age groups: under 5s, 5–19, 20–39, 40–64, 65+. The age profile for diabetes highlights the increasing mortality in each age group, with over two-thirds (69%) of all diabetes deaths among adults aged 65 and older. The years of full health lost because of diabetes is split evenly between adults aged 40–64 (49% of all healthy years lost) and adults aged 65+ (46% of all healthy years lost).
Regional inequalities
In 2019, the country with the lowest diabetes mortality rate in the region was Canada (7 deaths per 100 000), and would see 14 fewer deaths per 100 000 people than the regional average for the Americas (21 per 100 000), and 75 fewer deaths per 100 000 than the country with the highest mortality rate (Guyana, 83 per 100 000) (Figure 21). The overall regional diabetes inequality (IoD 107) was similar to that seen in prostate cancer (which in 2019 had the highest inequality of the top 10 cancer sites, IoD 105). The higher diabetes mortality rates were dominated by Caribbean countries. Among the 10 countries with the highest mortality rates in 2019 (mortality rate range 54 to 83 deaths per 100 000), seven were in the Caribbean.9
2.6 Mental and substance use disorders and neurological conditions
The global importance of mental health has been recognized by the inclusion of mental health and well-being in the Sustainable Development Goals.10 Many mental health disorders can be diagnosed and treated cost-effectively, and there is a growing recognition of the need for comprehensive mental health services to be offered as part of a universal health coverage (UHC) package (11). Yet in many parts of the world, mental health is still not acknowledged as important, has associated stigma, and remains a low health priority. Access to effective treatments remains limited. For example, according to WHO, only a quarter of countries worldwide have a national policy, strategy, or plan for supporting people with dementia (12).
Mental health and substance use disorders are a diverse group of conditions that can affect our thoughts, emotions, and behavior. Many conditions are on a spectrum of severity and at their most severe, can be life-threatening. Mental disorders include depression and anxiety, bipolar disorder, schizophrenia and other psychoses, and developmental disorders including autism. There are effective strategies for preventing some mental disorders, such as depression or anxiety. For most conditions there are effective treatments to alleviate the suffering they cause. Access to health care and social services capable of providing treatment and support is key.
Neurological conditions are diseases of the central and peripheral nervous system, and include epilepsy, Alzheimer disease and dementias, migraines and headache disorders, and Parkinson disease. There is a complex interplay between neurological conditions and mental health, and people living with a neurological condition suffer high levels of anxiety and depression. Although some mental and substance use disorders and neurological conditions (MHN) have important levels of associated mortality, most conditions are chronic and can lead to significant disability if untreated. This report section therefore puts a greater emphasis on disease burden, measured using DALYs.
Leading causes of death and disease burden
The absolute number of MHN deaths in the Americas increased from 235 000 in 2000 to 655 000 in 2019. Total deaths in the region increased by a smaller percentage, from 5.46 million in 2000 to 7.16 million in 2019, so that the share of deaths due to MHN increased markedly, from 4.3% in 2000 to 9.1% in 2019. The years of full health lost because of MHN in the Americas increased from 32.8 million in 2000 to 48.4 million in 2019. Total years of full health lost increased by a smaller percentage, from 249 million in 2000 to 296 million in 2019, so that the share of healthy years lost because of MHN increased from 13.2% in 2000 to 16.4% in 2019. The five leading causes of healthy years lost in the Americas in 2019 due to mental disorders and due to neurological conditions are summarized in Table 8.
General trends in mental health and substance use disorders and neurological conditions
MHN rates of disease rose consistently between 2000 and 2019. The mortality rate from mental and substance use disorders rose by 89% (from 5.9 to 11.1 deaths per 100 000) and the DALY rate rose by 10% (from 2877 to 3160 years per 100 000). The mortality rate from neurological conditions rose by 60% (from 20.5 to 32.9 deaths per 100 000) and the DALY rate rose by 15% (from 1125 to 1290 years per 100 000). MHN were the only group of conditions to report increases in mortality and disability rates; diabetes was the only other group of conditions to report a worsening disability rate in the 20 years from 2000. All other grouped causes reported mortality and disability rate improvements (improvements of between 5% and 33% for mortality rates, and improvements of between 10% and 29% for DALY rates).
Drug use disorders since 2000
Drug addiction, also called substance use disorder, affects a person's brain and behavior and leads to an inability to control the use of a legal or illegal drug or medication. This classification includes the misuse of opioids, cocaine, amphetamines, cannabis, sedatives and hypnotics, hallucinogens, and volatile solvents. Alcohol misuse is classified separately, and tobacco use is not part of this classification. Problems caused by drug addiction are classified into substance use disorders and substance induced disorders. Substance use disorders includes behaviors such as cravings to use the substance, wanting but failing to stop or cut down, taking a substance for longer and in larger amounts than intended, neglecting other daily activities, and continuing use when it harms health or relationships. Substance induced disorders includes things like intoxication, withdrawal, depression and anxiety, psychotic disorder, and sleep and sexual dysfunction. Drug use disorders in 2019 accounted for 1% of all deaths, and almost three-quarters (71%) of all mental and substance use disorder deaths in the Americas. The mortality rate from drug use disorders has increased since 2000, up by almost 200% (198%) to 8 deaths per 100 000 people. Although the increase has been greater among women (rising from 1.5 to 5.4 deaths per 100 000 among women – a 260% increase, and rising from 3.9 to 10.7 deaths per 100 000 among men – a 170% increase) there continues to be almost 2 deaths among men for every female death. Although the problem is region-wide, the United States had a mortality rate in 2019 of 21.3 deaths per 100 000, almost three times higher than the next highest national rate (Canada, 8.7 deaths per 100 000) and with 29 countries reporting a 2019 mortality rate of less than 2 deaths per 100 000. There was a similar profile for years of lost health, up from 387 years per 100 000 in 2000 to 782 per 100 000 in 2019, a rise of just over 100% (102%). The 20-year percentage increase was similar in women and men, with men maintaining a higher DALY rate in 2019 compared to women (DALY gender rate ratio 1.6). There were 4.8 million years of lost health among men in 2019, compared to 3.1 million lost years among women.
Notes: a Mortality is described using the age-standardized mortality rate. Disease burden is described using the age-standardized DALY rate. Both rates presented per 100 000 population. b Includes all mental and substance use disorders. Other conditions not listed include bipolar disorders, eating disorders, autism and Asperger syndrome, childhood behavioral disorders, and idiopathic intellectual disability. (All mental and substance use disorders ICD-10 codes: F04–F99, G72.1, Q86.0, X41–X42, X44, X45). c Includes all neurological conditions. Other conditions not listed include multiple sclerosis, cerebral palsy, motor neuron disease. (All neurological conditions ICD-10 codes: F01–F03, G06–G98, minus G14 and G72.1.)
Data source:World Health Organization. Mortality and global health estimates.
Alzheimer disease and dementias since 2000
The dementias are a group of related symptoms associated with an ongoing decline of brain functioning. There are many different causes of dementia, and many different types. Alzheimer disease and vascular dementia make up the majority of cases. Alzheimer disease is caused by a build-up of proteins (called plaques) and fibers (called tangles) in the brain that block nerve signals and destroy nerve cells. Vascular dementia is caused by reduced blood flow to the brain. Symptoms are similar and can include trouble remembering names, events, or conversations, problems concentrating, personality and mood changes, depression, impaired judgment and decision-making, and confusion. These problems can make daily activities increasingly difficult, and someone with the condition may eventually be unable to look after themselves. The slow disease progression makes this a distressing and debilitating condition for people living with the disease, and for their families. Alzheimer disease and the dementias in 2019 accounted for 5% of all deaths, and almost three-quarters (73%) of all deaths from neurological conditions in the Americas. The mortality rate from Alzheimer disease and dementias has increased dramatically since 2000, up by 89% to 22.3 deaths per 100 000 people. The 20-year increase has been the same in women and men, and the mortality rate remained slightly higher in women (mortality gender rate ratio 0.83). The older age profile of women compared to men means that there were many more deaths among women in 2019 (258 000 deaths among women, 133 000 deaths among men). There was a similar profile for years of lost health, up from 258 years per 100 000 in 2000 to 369 per 100 000 in 2019, a rise of 43%. The 20-year percentage increase was similar in women and men, with women maintaining a higher DALY rate in 2019 compared to men (DALY gender rate ratio 0.89). There were 3.6 million years of lost health among women in 2019, compared to 2.2 million lost years among men.
The mortality rate from Alzheimer disease and dementias has increased dramatically since 2000, up by 89% to 22.3 deaths per 100 000 people
Deaths across the life course
Figure 22 presents the proportion of deaths and DALYs in each of five age groups: under 5s, 5–19, 20–39, 40–64, 65+. Across all the mental and substance use disorders, over half (54%) of all deaths were among adults aged 40–64, with a further 30% among younger adults aged 20–39. This relatively young age profile was driven by the age profile of deaths from drug use disorders, with 51% of all deaths among adults aged 40–64 and 36% among adults aged 20–39. Most years of lost health due to the mental and substance use disorders were among young adults (aged 20–39, 14.5 million years lost, 44% of all healthy years lost) and older adults (aged 40–64, 11.7 million, 36%). Among the neurological conditions, deaths were almost exclusively among adults aged 65+ (90% of all deaths). Years of healthy life lost was still mostly among adults aged 65+ (7.5 million years lost, 48% of all healthy years lost). Healthy years were also lost among the younger age groups, because of the younger age profile of other neurological conditions: epilepsy, migraine, and non-migraine headaches.
Regional inequalities
Mental and substance use disorders. In 2019, the country with lowest DALY rate in the region was Colombia (1956 lost years of health per 100 000), and would see 1204 fewer DALYs per 100 000 people than the regional average for the Americas (3160 per 100 000), and 2734 fewer DALYs per 100 000 than the country with the highest DALY rate (United States, 4690 per 100 000) (Figure 23). The Colombia rate was 62% of the regional rate and 42% of the United States rate.
Neurological conditions. In 2019, the country with lowest DALY rate in the region was Argentina (842 lost years of health per 100 000), and would see 448 fewer DALYs per 100 000 people than the regional average for the Americas (1290 per 100 000), and 661 fewer DALYs per 100 000 than the country with the highest DALY rate (United States, 1503 per 100 000). The Argentina rate was 65% of the regional rate and 56% of the United States rate.
Overall, regional MHN inequalities were relatively low. The index of disparity (IoD) for mental and substance use disorders had risen from 20 in 2000 to 26 in 2019, and for neurological conditions it had risen from 11 in 2000 to 16 in 2019. These IoD values were driven by high DALY rates in the United States and to a lesser degree Canada, which in turn were dominated by high DALY rates for drug use disorders and for Alzheimer disease and the dementias. The IoD increases were due entirely to the substance use disorders (IoD increased from 59 to 80 between 2000 and 2019), and Alzheimer disease and the dementias (IoD increased from 27 to 35 between 2000 and 2019). All other leading causes of MHN reported a 20-year IoD decrease.
2.7 External causes
Injuries can result from a very wide range of external causes, with some of the more common events being road traffic collisions, falls, drowning, burns, poisoning, and acts of violence against oneself (known as self-harm) or by other people (known as interpersonal violence). Although there is strong evidence for what can help to prevent injuries and violence and to treat their consequences in various settings (13, 14), prevention can be complex, generally requiring sustained cooperation between different sectors of society. The prevention of violence and injuries cuts across several SDGs, including SDG targets 3.6 and 11.2 (both related to road safety), targets 4a (education), 5.2 (violence against women), 16.1 (all forms of violence), and 16.2 (all forms of violence against children) (15). In addition, a recent review has highlighted the broad relevance of the SDGs for injury prevention, recognizing (for example) that SDG efforts to promote gender equality, alleviate poverty, create safe cities and communities, and good health and well-being can all contribute to reducing the injury burden (16).
Leading causes of death and disease burden
The absolute number of deaths from injuries in the Americas increased from 524 000 in 2000 to 650 000 in 2019. Total deaths in the region increased by a slightly larger percentage, from 5.46 million in 2000 to 7.16 million in 2019, so that the share of deaths due to injuries fell slightly, from 9.6% in 2000 to 9.1% in 2019. The years of full health lost because of injuries in the Americas increased from 33.4 million in 2000 to 38.0 million in 2019. Total years of full health lost increased by a slightly larger percentage, from 249 million in 2000 to 296 million in 2019, so that the share of healthy years lost because of injuries fell slightly from 13.4% in 2000 to 12.8% in 2019. The five leading causes of healthy years lost in the Americas in 2019 due to injuries are summarized in Table 9.
General trends in injuries
Many more men were injured than women. Since 2000, the mortality and disability rates among men have remained three times higher than among women. In 2019 the injury mortality rate among men was 93 per 100 000 and among women it was 25 per 100 000 (a gender rate ratio of 3.7), and the injury disability (DALY) rate among men was 5538 per 100 000 and among women it was 1780 per 100 000 (a gender rate ratio of 3.1).
Injuries led to more years of lost health, relative to deaths, than most other conditions. In 2019 there were 58 years of lost health due to injuries for every injury death, and this compared to 20 years of lost health per death for cardiovascular diseases, 24 years per death for cancers, 27 years per death for respiratory disease, 29 years per death for neurological conditions, and 47 years per death for diabetes. Only mental and substance use disorders had a higher DALY to death ratio (268 years per death) because a number of the mental health conditions had no associated fatality.
Notes: a Mortality is described using the age-standardized mortality rate. Disease burden is described using the age-standardized DALY rate. Both rates are presented per 100 000 population. b All injuries includes other injuries, such as poisonings, fire and heat, exposure to mechanical forces, natural disasters, and collective violence and legal intervention. (All injuries ICD-10 codes: V01–Y89, minus X41–X42, X44, and X45.)
Data source:World Health Organization. Mortality and global health estimates.
Interpersonal violence since 2000
Interpersonal violence includes any injury inflicted by another person with intent to injure or kill, by any means. The definition excludes injuries inflicted by law-enforcing agents in the course of legal operations, and injuries due to operations of war, both of which are recorded separately. Although further classification of interpersonal violence (to identify, for example, intimate partner violence) is crucial for planning prevention programs, this additional detail is not available from the WHO Global Health Estimates (GHE) data. Interpersonal violence in 2019 accounted for 3% of all deaths and almost one-third (30%) of all injury deaths in the Americas. The mortality rate from interpersonal violence decreased slightly since 2000, down by 3% to 19 deaths per 100 000 people, with similar reductions in women and men. The mortality rate remained far higher among men in 2019, with 33.6 deaths per 100 000 among men compared to 4.7 deaths per 100 000 among women; there was a consistent excess of deaths among men in the 20 years since 2000 – always between 6 and 7 deaths among men for every female death. There was a similar profile for years of lost health, down marginally from 1172 years per 100 000 in 2000 to 1123 per 100 000 in 2019, a fall of just 4%. Men lost many more years of full health in 2019 compared to women (DALY gender rate ratio 6.5). There were 9.7 million years of lost health among men in 2019, compared to 1.5 million lost years among women.
Road injuries since 2000
The SDGs set an ambitious target of halving road traffic fatalities and injuries by 2020 (SDG Target 3.6) (17). Road traffic collisions disproportionately affect vulnerable road users, with more than half of deaths among pedestrians, cyclists, and motorcyclists. Road traffic injuries can be prevented, but this is not easy. It requires a safe systems approach with multisectoral involvement from transport, police, health, education, and actions that address the safety of roads and vehicles, safer use of roads, and an adequate/opportune post-crash response (18). Road traffic collisions in 2019 accounted for 2% of all deaths and almost one-quarter (24%) of all injury deaths in the Americas. The mortality rate from road traffic injuries has decreased since 2000, down by 15% to 14 deaths per 100 000 people, with larger reductions in women compared to men. The mortality rate remained far higher among men in 2019, with 22.9 deaths per 100 000 among men compared to 6.3 deaths per 100 000 among women; there was a consistent excess of deaths among men in the 20 years since 2000 – rising from 3.2 to 3.7 male deaths for every female death. SDG 3.6 required a 50% reduction in fatalities between 2010 and 2020. Mortality rates in 2010 were 25.2 per 100 000 among men and 7.1 per 100 000 among women. By 2019, mortality rates had fallen by 9% among men and by 12% among women.
Self-harm since 2000
Intentional self-harm is a broad classification for any purposely self-inflicted poisoning or injury. Most acts of self-harm are rooted in extreme emotional distress, and may be impulsive. Common causes of self-harm and suicide include: mental disorders such as depression, alcohol or substance abuse, feelings of desperation from a personal crisis, experiencing long-standing isolation, prejudice, or discrimination, or experiencing physical, emotional, or sexual abuse. Although most people who self-harm do not intend to kill themselves, the results can be fatal. Having access to dangerous means such as pesticides, pills, or guns increases the risk of someone hurting or killing themselves (19). Self-harm in 2019 accounted for 1.4% of all deaths and 15% of all injury deaths in the Americas. The mortality rate from self-harm has increased since 2000, up by 16% to 9 deaths per 100 000 people, with larger increases in women compared to men. The mortality rate remained higher among men in 2019, with 14.2 deaths per 100 000 among men compared to 4.1 deaths per 100 000 among women; there was a consistent excess of deaths among men in the 20 years since 2000 – falling from 3.9 to 3.5 male suicides for every female suicide. There was a similar profile for years of lost health, up from 370 years per 100 000 in 2000 to 441 per 100 000 in 2019, an increase of 19%, with a 27% increase among women compared to a 16% increase among men. Men lost more years of full health in 2019 compared to women (DALY gender rate ratio 3.2). There were 3.4 million years of lost health among men in 2019, compared to 1.1 million lost years among women.
Falls since 2000
A fall is an event that results in a person coming to rest inadvertently on the ground or floor or other lower level. Falls, trips, and slips can occur on one level or from a height (20). Although falls are a public health concern throughout the life course, many more falls occur among adults aged 65 and older. Public health progress at reducing the occurrence of falls and the severity of outcomes must tackle complex interrelationships between a person's physical health, their behavior, their physical environment, and their cultural and socioeconomic environment. Recently, a systems approach has been advocated that moves beyond individual behavior and provides for environments, policies, and awareness that prioritize safety, creating buffers so that falls are either avoided or made less serious because of protections in place (21). Falls in 2019 accounted for 1.1% of all deaths and 12% of all injury deaths in the Americas. The mortality rate from falls has increased markedly since 2000, up by 51% to 5.4 deaths per 100 000 people, with larger increases in women compared to men. The mortality rate remained higher among men in 2019, with 7.1 deaths per 100 000 among men compared to 3.9 deaths per 100 000 among women; there was a small excess of deaths among men in the 20 years since 2000 – falling from 2.3 to 1.8 male deaths for every female death. There was a similar profile for years of lost health, up from 382 years per 100 000 in 2000 to 410 per 100 000 in 2019, an increase of 7%, with a 15% increase among women compared to a 3% increase among men. Men lost more years of full health in 2019 compared to women (DALY gender rate ratio 1.5). There were 2.7 million years of lost health among men in 2019, compared to 2.3 million lost years among women.
Deaths across the life course
Unlike the other broad causes of disability and death,11 injuries can affect people across the life course. Four of the five leading causes of injury (injuries due to falls is the exception) have their highest proportion of deaths and disability among young adults aged 20–39 (Figure 24). This is particularly apparent for the leading cause of injury – interpersonal violence – where 52% of all deaths and 57% of all healthy years lost are among young adults, 24 percentage points and 35 percentage points higher than the next most common age group – adults aged 40–64. Indeed among children and adolescents (aged 5–19 years) the leading five causes of death include12 interpersonal violence (25% of all deaths in this age group), road injuries (16%), self-harm (7%), and drowning (4%), with leukemia being the only non-injury-based cause of death among the top five causes. The situation is similar for young adults (aged 20–39 years), with the leading five causes of death being interpersonal violence (23% of all deaths in this age group), road injuries (12%), self-harm (8%), and drug use disorders (7%), with ischemic heart disease being the only non-injury-based cause of death among the top five causes.
While deaths from interpersonal violence often spike in young adulthood, it is noteworthy that children first engage with violent behaviors much earlier in the life course, thus requiring intervention much earlier. This may include preventing intimate partner violence against women, thereby reducing the likelihood that children witness violence in their homes, or reducing child maltreatment in the early years.
Regional inequalities
In 2019, the country with lowest injury mortality rate in the region was Canada (27 deaths per 100 000), and would see 32 fewer injury deaths per 100 000 people than the regional average for the Americas (59 per 100 000), and 109 fewer injury deaths per 100 000 than the country with the highest mortality rate (Guyana, 136 per 100 000) (Figure 25). Country inequalities due to interpersonal violence (IoD 83) and drowning (IoD 110) were particularly high. The high inequality for drowning was driven by a small group of small island developing states (SIDS), with mortality rates ranging from 18 deaths per 100 000 (in Guyana) to 4.8 per 100 000 (in Suriname). All other countries had a mortality rate below 4 per 100 000, and 13 countries had rates below 2 per 100 000. The high inequality for interpersonal violence was driven by particularly high mortality rates in El Salvador (87 deaths per 100 000 in 2019), Honduras (81 per 100 000), Venezuela (Bolivarian Republic of) (65 per 100 000), Jamaica (48 per 100 000), and Belize (40 per 100 000).
2.8 Summary of key messages
Grouped causes
- Six grouped causes of death and disability were considered: cardiovascular diseases, cancers, respiratory diseases, diabetes, mental and substance use disorders and neurological conditions, and external causes (also known as injuries from unintentional and intentional causes).
- For the entire 20-year period, deaths in the Americas have been dominated by cardiovascular diseases and cancers, which in 2019 collectively accounted for 47% of all regional deaths.
- Mental and substance use disorders and neurological conditions accounted for 16% of all healthy years of life lost – more than the healthy years lost to cardiovascular diseases (14%) or injuries (13%).
- Among women the most important cause of death in 2019 was cardiovascular diseases (29% of all female deaths), and the most important cause of disability was mental and substance use disorders and neurological conditions (18% of all female disability-adjusted life years, DALYs).
- Among men the most important cause of death in 2019 was cardiovascular diseases (27% of all male deaths), and the most important cause of disability was external causes, otherwise known as injuries (18% of all male DALYs).
- The relative importance of diabetes, and of mental and substance use disorders and neurological conditions as regional causes of lost life and lost health increased in the Americas between 2000 and 2019.
Individual causes
- The six groups of lost life and lost health can be divided into 57 individual causes.
- Ischemic heart disease (IHD), strokes, and chronic obstructive pulmonary disease (COPD) have dominated regional deaths for the 20-year period since 2000.
- The relative importance of Alzheimer disease and dementias, drug use disorders, and injury from falls as causes of lost life increased markedly between 2000 and 2019.
- Eight different cancers were in the top 20 causes of death, with the top five cancers being trachea, bronchus, and lung cancers (7th position), breast cancer (8th position), prostate cancer (9th position), colorectal cancer (12th position), and cervical cancer (15th position).
- IHD was also the leading cause of disease burden, measured using DALYs.
- Some illnesses did not feature as a cause of death but were important causes of disease burden, notably depressive disorders (7th most important cause of disease burden), anxiety disorders (9th position), alcohol use disorders (14th position), and migraines (15th position).
- Five illnesses gained importance as causes of lost years of health in the 20 years since 2000: Alzheimer disease and dementias (rising from 20th to 16th most important cause of lost health), self-harm (16th to 11th), drug use disorders (12th to 6th), diabetes (5th to 3rd), and interpersonal violence (3rd to 2nd).
Cardiovascular diseases
- The five leading causes of cardiovascular disease (CVD) deaths in 2019 were ischemic heart disease (IHD), stroke, hypertensive heart disease; cardiomyopathy, myocarditis and endocarditis, and rheumatic heart disease.
- IHD – the most common CVD – in 2019 accounted for 15% of all regional deaths among women and men combined, and over half (54%) of all CVD deaths in the Americas.
- After IHD, stroke was the second most common CVD condition. In 2019, the regional stroke burden was roughly half that of IHD, with 478 000 deaths and 10.3 million years of lost health.
- For four of the five leading causes of CVD (hypertensive heart disease was the exception), there were important reductions in death and DALY rates. For women and men combined, the reductions ranged from 35% to 45% for death rates, and from 31% to 34% for DALY rates.
- These rate reductions were generally not large enough to offset the region's increasing population, and its rapid aging, so that the overall numbers of CVD deaths and years of lost healthy life continued to increase.
- Again, for four of the five leading causes of CVD (rheumatic heart disease was now the exception), men were disproportionately affected by CVD, with a higher burden of deaths and DALYs. In 2019, the ratio of male to female death rates ranged from 1.18 to 1.80, and the range for DALY rates was 1.14 to 2.03.
- For IHD, stroke, and hypertensive heart disease, around three-quarters of all deaths and two-thirds of the disease burden were among adults aged 65 and older.
- There was wide variation in mortality between countries. The absolute difference between the lowest and highest country mortality rates for each cause of CVD death was for IHD (156 additional deaths per 100 000 people), stroke (148 additional deaths per 100 000), hypertensive heart disease (51 additional deaths per 100 000), cardiomyopathy, myocarditis, and endocarditis (13 additional deaths per 100 000), and rheumatic heart disease (9 additional deaths per 100 000).
Cancers
- The five cancer sites with the highest associated mortality rates in 2019 were lung cancer, breast cancer, prostate cancer, colorectal cancer, and cervical cancer.
- Cancers of the trachea, bronchus, and lung were the most common cause of cancer death and disability in women and men combined – in 2019 these accounted for 4% of all deaths in the Americas and 19% of all cancer deaths. These caused 256 000 deaths and 5.5 million years of lost health.
- Despite a sustained drop in mortality rate, lung cancer remained the leading cause of cancer death and disability between 2000 and 2019.
- Among women in 2019, breast cancer was the most important cause of cancer death, with a mortality rate of 16 per 100 000 women. It caused 108 000 deaths among women and 3.1 million years of lost health.
- Among men in 2019, prostate cancer was the second most important cause of cancer death, with a mortality rate of 15 per 100 000 men. It caused 98 000 deaths among men and 1.8 million years of lost health.
- For eight of the 10 leading causes of cancer (liver and pancreatic cancers were the exceptions), there were important reductions in death and DALY rates. For women and men combined, the reductions ranged from 19% to 33% for death rates and from 16% to 37% for DALY rates.
- These rate reductions were not large enough to offset the region's increasing population, and its rapid aging, so that the overall number of cancer deaths and years of lost healthy life continued to increase.
- Aside from the sex-specific cancers (breast, prostate, cervical), men were disproportionately affected, with a higher burden of deaths and DALYs. In 2019, the ratio of male to female death rates ranged from 1.27 to 1.79, and the range for DALY rates was 1.31 to 1.80.
- Among the 10 leading causes of cancer deaths, cervical and prostate cancer had the largest mortality rate inequalities between countries of the Americas, perhaps reflecting differences in the coverage of screening programs, and for cervical cancer, vaccination coverage.
- Caribbean countries dominate the highest mortality rates for breast and prostate cancer, perhaps partly reflecting the genetic basis of aggressive disease among populations of African descent.
Respiratory diseases
- The two leading causes of respiratory disease (RD) deaths in 2019 were chronic obstructive pulmonary disease (COPD) and asthma.
- COPD primarily affects older adults, whereas asthma leads to years of full health lost across the life course.
- In 2019 there were 378 000 COPD deaths, 5% of all deaths, and almost three-quarters (71%) of all RD deaths in the Americas.
- The COPD mortality rate improved since 2000, down by 18% to 25 COPD deaths per 100 000 people.
- This 20-year COPD improvement has been much greater in men than women. The mortality rate among men improved by 27%, compared to 10% among women.
- Mortality from asthma is low and falling. In 2019 there were 13 000 asthma deaths, with the mortality rate falling by 47% since 2000.
- Country mortality rates for COPD ranged from 7 to 49 deaths per 100 000, and for asthma they ranged from 0.4 to 13 deaths per 100 000.
Diabetes
- In 2019 there were 284 000 diabetes deaths, 4% of all deaths in the Americas, up from 178 000 deaths in 2000.
- The diabetes mortality rate improved slightly since 2000, down by 5% to 21 diabetes deaths per 100 000 people.
- There was a dramatic increase in the years of full health lost because of diabetes, up from 7.2 million years in 2000 to 13.4 million years in 2019.
- In 2019 men had a higher diabetes mortality rate and DALY rate compared to women across the region (rate ratio 1.2 in both cases).
- These gender ratios were at parity in 2000, highlighting a consistent 20-year trend toward a worse diabetes burden among men.
- The higher diabetes mortality rates were dominated by Caribbean countries. Among the 10 countries with the highest mortality rates in 2019 (mortality rate range 54 to 83 deaths per 100 000), seven were in the Caribbean.
Mental and substance use disorders and neurological conditions
- The number of deaths due to mental and substance use disorders and neurological conditions (MHN) in the Americas increased from 235 000 in 2000 to 655 000 in 2019, an increase of 179%.
- The years of full health lost because of MHN in the Americas increased from 32.8 million in 2000 to 48.4 million in 2019, an increase of 47%.
- MHN were the only group of conditions to report increasing mortality and disability rates between 2000 and 2019.
- Among mental and substance use disorders, mortality rates rose by 89% and disability (DALY) rates rose by 10%.
- Among neurological conditions, mortality rates rose by 60% and disability rates rose by 15%.
- Mental and substance use disorders were dominated by drug use disorders, which accounted for almost three-quarters (71%) of all deaths and one-quarter (24%) of all years of lost health.
- Drug use disorders were dominated by rates in the United States with a mortality rate of 21.3 deaths per 100 000, almost three times higher than the next highest national rate (Canada, 8.7 deaths per 100 000).
- Neurological conditions were dominated by Alzheimer disease and the dementias, which accounted for three-quarters (73%) of all deaths and over one-third (37%) of all years of lost health.
- Alzheimer disease and the dementias were dominated by rates in the United States and Canada with a mortality rate of 33 and 28 deaths per 100 000, respectively, compared to the third highest value (Suriname) of 24 deaths per 100 000.
External causes
- The absolute number of deaths from injuries in the Americas increased from 524 000 in 2000 to 650 000 in 2019.
- Many more men were injured than women. Since 2000, the mortality and disability rates among men have remained three times higher than women.
- Interpersonal violence in 2019 was the leading cause of injury in the Americas, accounting for 3% of all deaths and almost one-third (30%) of all injury deaths in the Americas.
- Road injuries, self-harm, falls, and drowning made up the top five causes of injury deaths in the Americas in 2019.
- Four of the five leading causes of injury (injuries due to falls is the exception) have their highest proportion of deaths and disability among young adults aged 20–39. Intervention at earlier ages is important to prevent the deaths and injuries in this age group.
- Across the Region, mortality rates fell between 2000 and 2019 for interpersonal violence (3% drop), road injuries (15% drop), and drowning (32% drop). Mortality rates increased for self-harm (16% increase) and for falls (51% rise).
Footnotes
3 The World Health Organization (WHO) regions are: Africa, The Americas, Eastern Mediterranean, Europe, South-East Asia, and Western Pacific.
4 The Pan American Health Organization (PAHO) subregions are: North America, Southern Cone, Central America, Andean, Latin Caribbean, non-Latin Caribbean, Brazil, and Mexico.
5 This restriction to cardiovascular diseases, cancers, respiratory diseases, diabetes, mental and substance use disorders and neurological conditions, and injuries means that certain leading causes of mortality and disease burden are not in this top 20; for example, lower respiratory infections,neonatal conditions, kidney diseases, and cirrhosis of the liver.
6 Throughout this report, diabetes is defined as ICD-10 codes E10–E14 (minus E10.2, E11.2, E12.2, E13.2, E14.2). This classification includes insulindependent diabetes, non-insulin-dependent diabetes, malnutrition-related diabetes. It does not include diabetes arising in pregnancy (gestational diabetes) or diabetes-related renal complications (these are included in a separate categorization of kidney diseases).
7 This statement applies to cancer mortality and disability rates for women and men combined. For women alone, breast cancer has a higher disease burden (measured using mortality and disability rates). For men alone, lung cancer is the leading cancer.
8 Throughout this report, diabetes is defined as ICD-10 codes E10–E14 (minus E10.2, E11.2, E12.2, E13.2, E14.2). This classification includes insulindependent diabetes, non-insulin-dependent diabetes, and malnutrition-related diabetes. It does not include diabetes arising in pregnancy (gestational diabetes) or diabetes-related renal complications (these are included in a separate categorization of kidney diseases).
9 The 10 countries with the highest diabetes mortality rate in 2019 were: Guyana (83 per 100 000), Mexico (72), Trinidad and Tobago (70), Haiti (68),Grenada (65), Guatemala (63), Jamaica (62), Saint Lucia (59), Belize (54), and Suriname (54).
10 The Sustainable Development Goal 3.4 target states: “by 2030 reduce by one-third premature mortality from non-communicable diseases (NCDs) through prevention and treatment and promote mental health and well-being.” Within this target, indicator 28 requires the reporting of the “Proportion of persons with a severe mental disorder (psychosis, bipolar affective disorder, or moderate-severe depression) who are using services”.
11 These six broad causes are: cardiovascular diseases, cancer, respiratory diseases, diabetes, mental and substance use disorders and neurological conditions, and injuries.
12 These leading five causes in each age group are from among the six groups of causes considered in this report: cardiovascular diseases, cancers, respiratory diseases, diabetes, mental and substance use disorders and neurological conditions, and injuries.