Sepsis is a complication that arises when the human body mounts an indiscriminate, and overt, response to an infection. Sepsis is a medical emergency. If not diagnosed and treated early, sepsis can lead to irreversible tissue damage, septic shock, multiple organ failure and potentially death. Septic shock is a severe type of sepsis in which the circulatory, cellular, and metabolic abnormalities are associated with a greater risk of mortality than with sepsis alone.
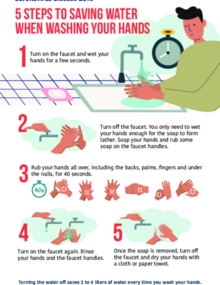
- Approximately 70% of health care workers and 50% of surgical teams do not routinely practice hand hygiene.
- Hand hygiene saves millions of lives every year when performed at the right times in health care.
- The burden of sepsis is highest in low and middle-income countries, where it represents a major cause of maternal and neonatal morbidity and mortality. However, estimating the precise global epidemiological burden of sepsis is difficult, due to limitations in diagnosis and reporting.
- Each year, approximately 31 million people have an episode of sepsis. Of these, about 6 million people die from sepsis. In low and middle income countries the burden of sepsis is higher and represents one of the leading causes of maternal and neonatal death. Despite this, it is very difficult to assess the burden of disease worldwide due to limitations in diagnosis and notification.
- The occurrence, frequency, and fatality of sepsis are determined by complex interplaying factors including host immunity, causative pathogen, timely diagnosis, and access to quality care. Most sepsis occurs as a complication of common preventable infections in the community (community-acquired infection). It also frequently results from infections acquired in healthcare settings, especially among immunocompromised patients. Healthcare-acquired infections are often resistant to antibiotics. This makes the management of these infections challenging, and are often associated with poor patient outcome; and higher economic burden.
- Sepsis is frequently undetected and/or misdiagnosed, during initial onset when it is effectively treatable. Increasing awareness of the clinical manifestations of sepsis in the community, building capacity for early detection, appropriate timely management, and reporting, are some of the major challenges facing effective prevention and control of sepsis.
PAHO aims to include prevention, diagnosis and treatment of sepsis in national health systems strengthening communities and health care settings, according to WHO guidelines; to reinforce existing strategies or develop new ones leading to strengthened infection prevention and control programs, including by strengthening hygienic infrastructure, promoting hand hygiene, and other infection prevention and control best practices, clean childbirth practices, infection prevention practices in surgery, improvements in sanitation, nutrition and delivery of clean water, access to vaccination programmes and provision of effective personal protective equipment for health professionals and infection control in health care settings.