Infection from rotavirus is the most common cause of diarrhea among children under five years old worldwide.
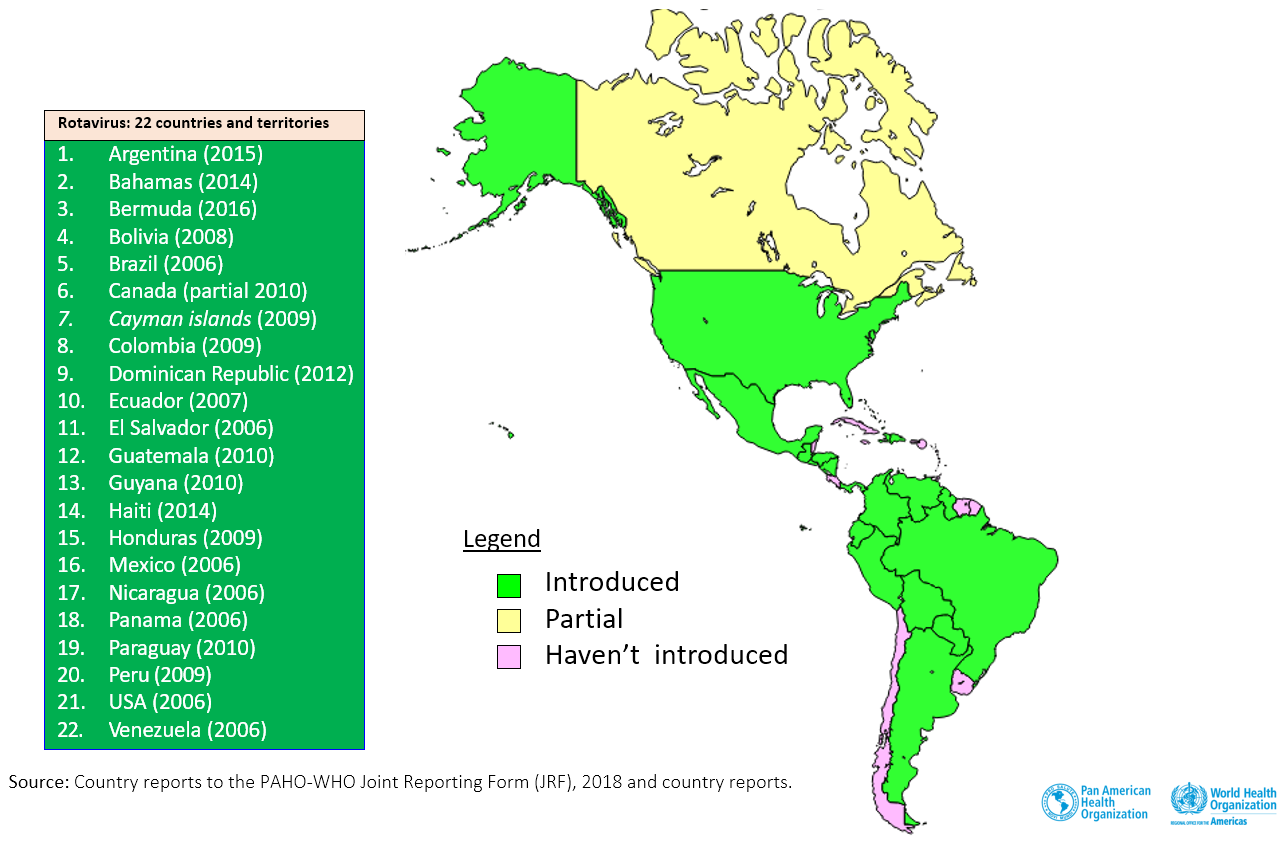
In 2016, it was estimated that the number of rotavirus deaths in children under 5 years of age declined from 528 000 (range, 465 000–591 000) in 2000 to 215 000 (range, 197 000–233 000) in 2013 worldwide. In 2018 in Latin American and Caribbean, reductions of 64.0% were observed in rotavirus hospitalizations, 32.8% in acute gastroenteritis (AGE) hospitalizations, and 53.5% in AGE-related mortalities in children under 5 years. In 2015, an estimated 125,000 rotavirus-associated hospitalizations and 800 rotavirus-related deaths were prevented in countries that implemented rotavirus vaccines in the Region.
While the incidence of rotavirus infection in High-income and Low-Middle-Income-Countries is similar, 80% of deaths occur in developing countries.
Four countries (India, Nigeria, Pakistan, and Democratic Republic of Congo) accounted for approximately half (49%) of all estimated rotavirus deaths in 2013.
Since the virus tends to spread through contaminated hands, all family members and personnel at health and day care centers should wash their hands after cleaning a child who has defecated, after disposing of the child’s stool after defecating, before preparing food, before eating, and before feeding a child.
Although improvements in hygiene, water supply, and wastewater elimination are all measures that can help to reduce severe episodes of diarrhea, comparable incidences of rotavirus disease in developed and developing countries indicate that the disease cannot be controlled exclusively with such measures.
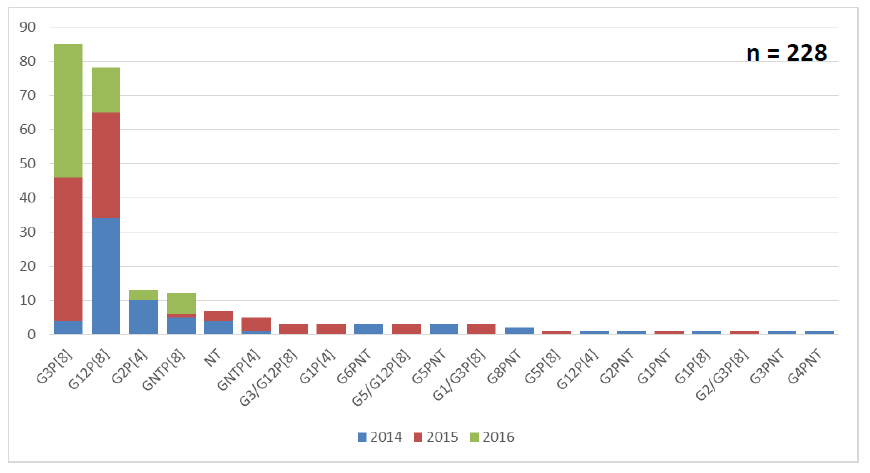
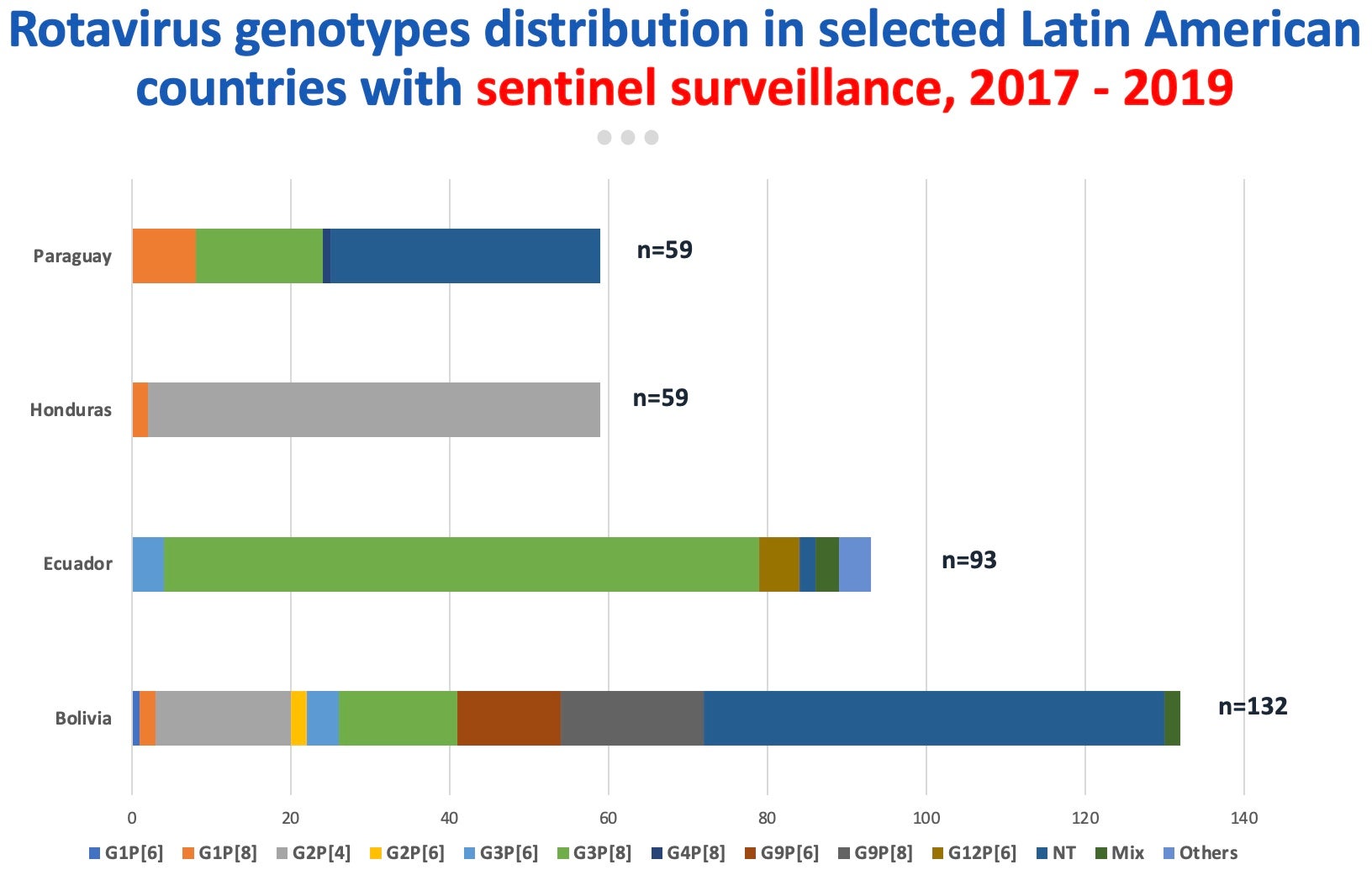
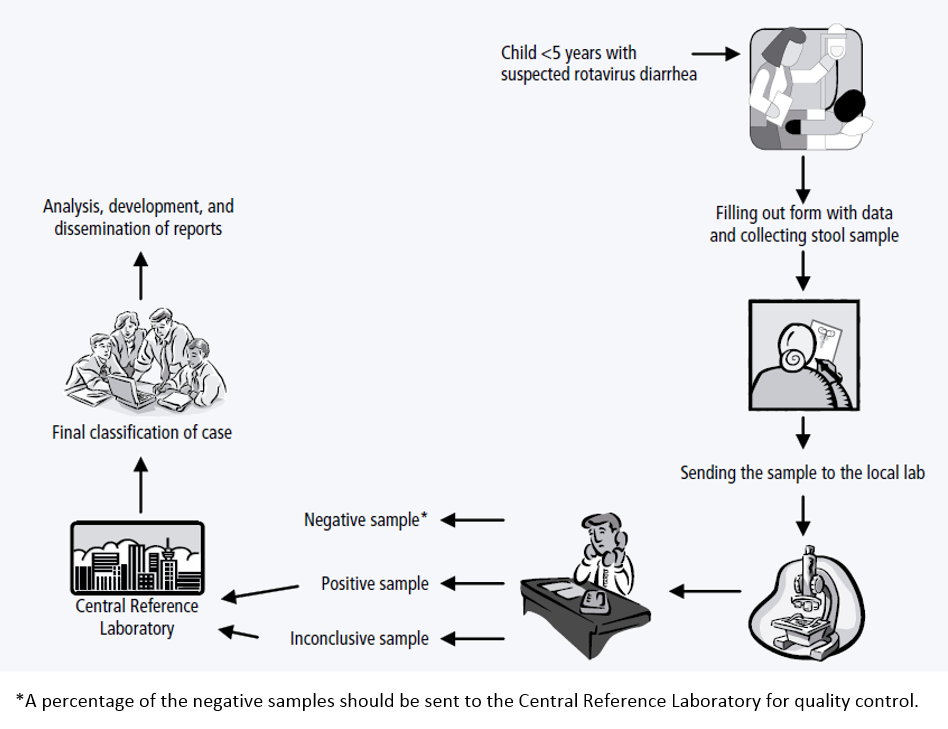
PAHO’s rotavirus sentinel surveillance network began in 2006. In the beginning, the data collected was aggregated, but since 2014 when the regional network integrated the WHO Global Sentinel Surveillance Network, the collection has been case-by-case using the VINUVA case data system. Currently, seven countries and 16 hospitals are included in this network.
PAHO’s Technical Advisory Group (TAG) on Vaccine-preventable Diseases recommends that countries in the Region of the Americas should continue making efforts to administer rotavirus vaccines as part of their routine immunization schedules, at the recommended ages, usually at 2 and 4 months or 2, 4 and 6 months.