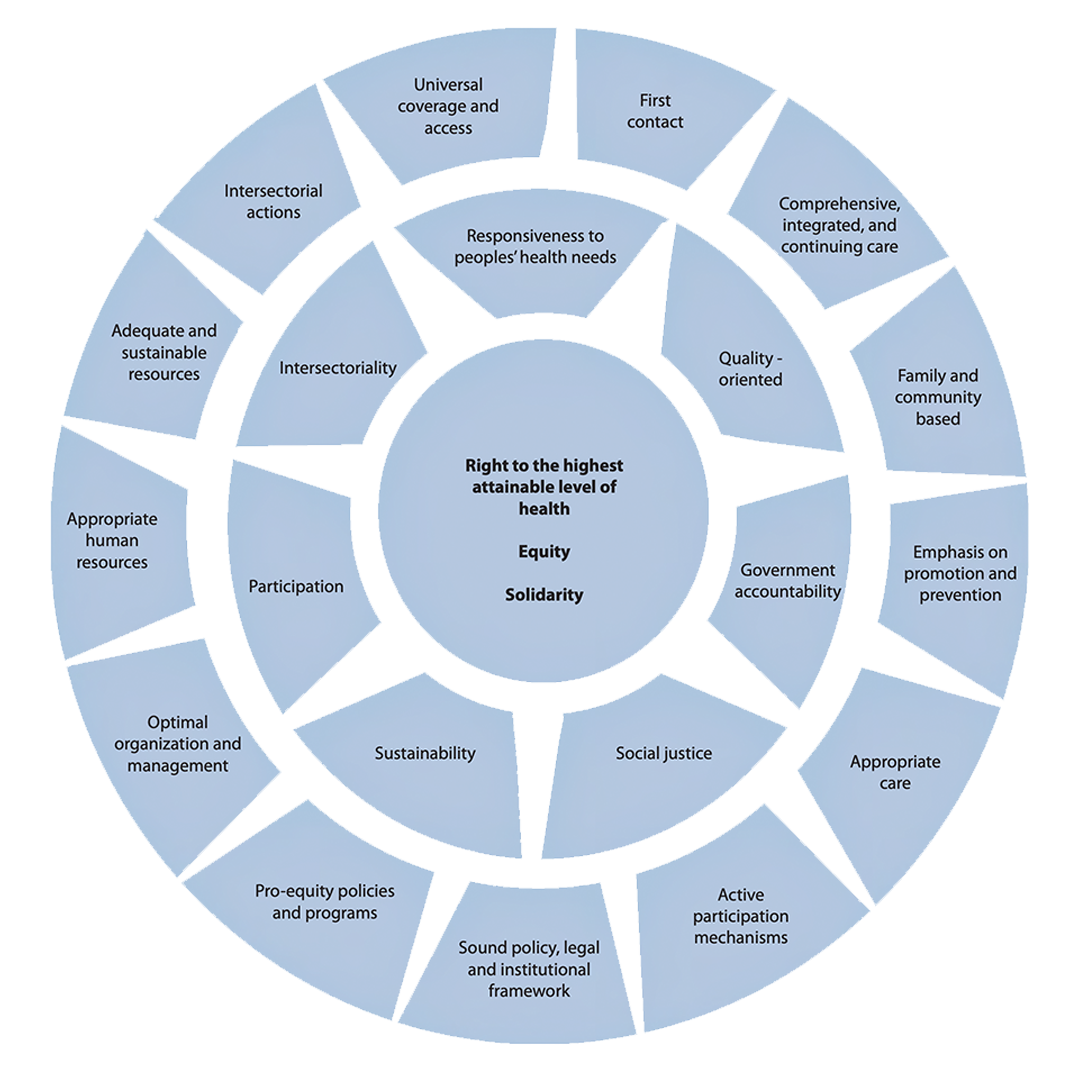
PAHO considers Integrated health services networks as one of the principal operational expressions of Primary Health Care-based health systems at the health services level, helping to make several of its most essential elements a reality such as universal coverage and access, first contact,comprehensive, integrated and continuing care, appropriate care, optimal organization and management, family and community orientation, and intersectoral action, among others.
- The purpose of the PAHO Initiative on Integrated Health Service Delivery Networks (IHSDNs) is to contribute to the development of PHC-based health systems, and thus to health services delivery that is more accessible, equitable, efficient, of higher technical quality, and that better fulfills citizens’ expectations
- PAHO considers IHSDNs as one of the principal operational expressions of PHC-based health systems at the health services level, helping to make several of its most essential elements a reality such as universal coverage and access, first contact, comprehensive, integrated and continuing care, appropriate care, optimal organization and management, family and community orientation, and intersectoral action, among others
List of Essential Attributes of Integrated Health Service Delivery Networks (IHSDNs)
- Clear definiton of the populations/territory covered and extensive knowledge of the health needs and preferences of this population, which determines the supply of health services
- An extensive network of health care facilities that offers health promotion, disease prevention, diagnosis treatment, disease-management, rehabilitation and pallative care, and that integrates programs targeting specific diseases, risks and populations, as well as personal and public health services.
- A multi-diciplinary first level of care that covers the entire population, serves as a gateway to the system, and integrates and coordinates health care, in addition to meeting most of the population's health needs
- Delivery of specialized services at the most appropiate locartion, preferably in non-hospital settings
- Existence of mechanisms to coordinate health care throughout the health service continuum
- Care that is person-, family- and community-centered and that takes into account cultural and gender-related characteristics and diversity
- A unified system of governance for the entire network
- Borad social participation
- Intersectoral action that addresses wider determinants of health and equity in health
- Integrated management of clinical, administrative and logistical support systems
- Sufficient, competent and committed human resources for health that are valued by the network
- An integrated information system that links all network members with data disaggregated by sex, age, place of residence, ethnic origin, and other pertinent variables
- Result-bases managemnt
- Adequate funding and financial incentives aligned with networks goals
Fragmentation of health services is a major cause of poor performance of health services, and thus of the underperformance of health systems in general. Fragmentation can generate, on its own, or combined with other factors, difficulties in access to services, delivery of services of poor technical quality, irrational and inefficient use of available resources, unnecessary increases in production costs, and low user satisfaction with services received.
In response to the challenges posed by health services fragmentation and to various international mandates and commitments, PAHO/WHO is developing the initiative on Integrated Delivery Networks (IDN) with a view to contribute to the strengthening of Health Systems based on Primary Health Care (PHC), and thus to the delivery of more accessible, equitable, efficient, and quality health services that better meet the expectations of the population.