Each year, disasters cost between US$300-500 billion worldwide, with disproportionate effects on low-income countries. The Americas are the second continent most affected by disasters. Almost a fourth of all disasters that occurred in the world in 2017 took place somewhere in the Americas, representing cumulative damages of approximately US$ 306 billion.
Therefore, the need for comprehensive preparedness of the health sector. For that, a more effective surveillance and a collective rapid response in the Latin America and Caribbean (LAC) Region is required to respond to potential pandemics, outbreaks, more frequent and destructive natural disasters, and conflicts.
Overall, the capacity of LAC countries to manage the response to a minor emergency or small-scale disaster, without seeking aid from the international community, has increased. However, there is a growing demand for different levels of technical cooperation with increased specificity to countries’ particular needs, or to respond to large multi-hazard emergencies, particularly when national capacities are overwhelmed.
In September 2016, the Plan of Action for Disaster Risk Reduction (DRR) 2016-2021 was approved by the Ministers of Health of the Americas, aligned with key recent international instruments including the 2030 Agenda for Sustainable Development, the Paris Agreement on Climate Change and the Sendai Framework for Disaster Risk reduction 2015-2030.
The purpose of the plan is to continue strengthening disaster risk reduction in order to prevent deaths, diseases, disabilities, and the psychosocial impact of emergencies and disasters through people-centered actions and cross-cutting approaches. The plan aims to improve the safety of integrated health services networks through the application of safe hospital criteria and approaches to climate change in the planning, design, construction and operation of such services.
- The annual losses caused by earthquakes, tsunamis, cyclones, winds, and tidal waves are estimated to represent between 1.2% and 1.7% of the world’s gross domestic product (GDP).
- The most common events were of hydrological and meteorological type, which caused the highest percentage of deaths and damages in this period.
- More than half of the 16,000 hospitals in Latin America and the Caribbean are in areas at high risk for disasters.
-
Climate change means higher average temperatures are recorded each year, and more people are being affected by disasters, climate-sensitive diseases and other health conditions.
PAHO’s work in disaster risk reduction and response is carried out in an environment of cooperation, in which Member States, health authorities, sub-regional organizations and a wide variety of other strategic partners work together to achieve a more resilient health sector in the Americas and help reduce the health consequences of emergencies, disasters and crises and ease their social and economic impact.
The Disaster Risk Reduction unit of the Health Emergencies Department supports countries in the implementation of the Plan of Action on Disaster Risk Reduction 2016 – 2021, which aims to protect the lives of patients and health workers, shield health equipment and supplies from disasters, and ensure that the health services continue operating effectively during and after emergencies and disasters in order to save lives, reduce disabilities, and enable the health sector to fulfill its continuing responsibilities.
The PAHO PHE DRR area also works in the implementation of the Plan of Action on Safe Hospitals 2010-2015. This plan has contributed to the adoption of national programs and policies for safe hospitals, to the implementation of activities aimed at ensuring that all new hospitals are built with a higher level of protection and to the implementation of measures to cope with climate change in terms both of disaster adaptation and mitigation in order to strengthen existing health facilities.
Additional work under the scope of the DRR area:
- Promotion and implementation of climate-smart mitigation and adaptation measures for health facilities;
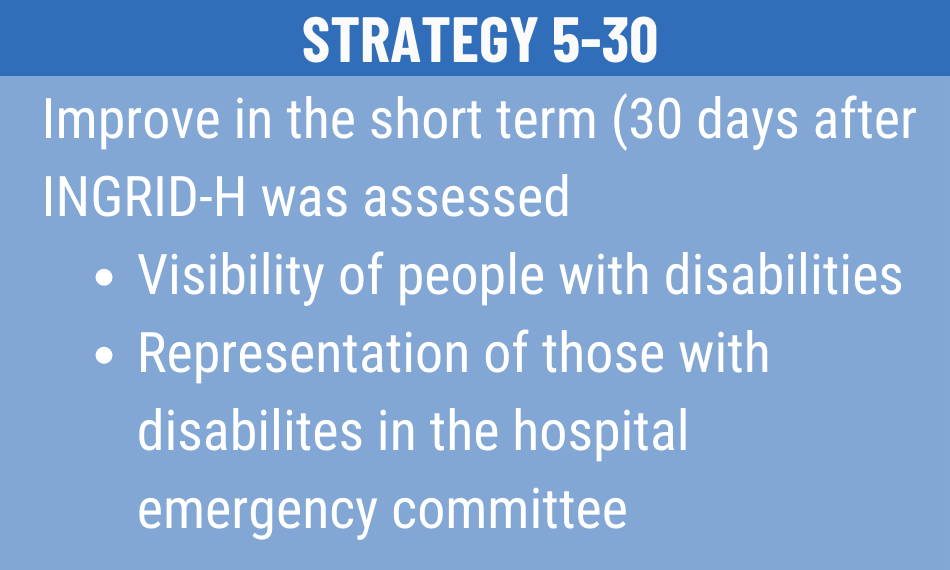
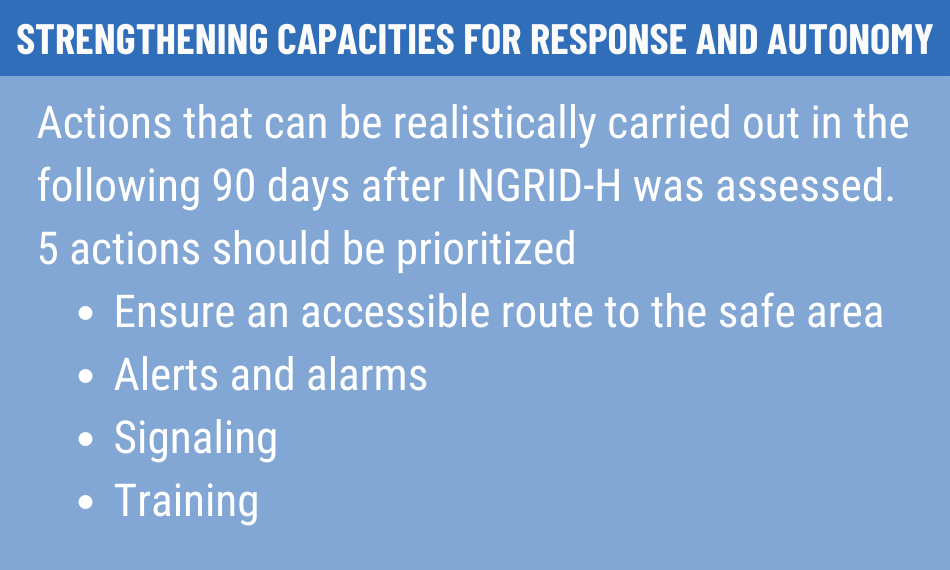
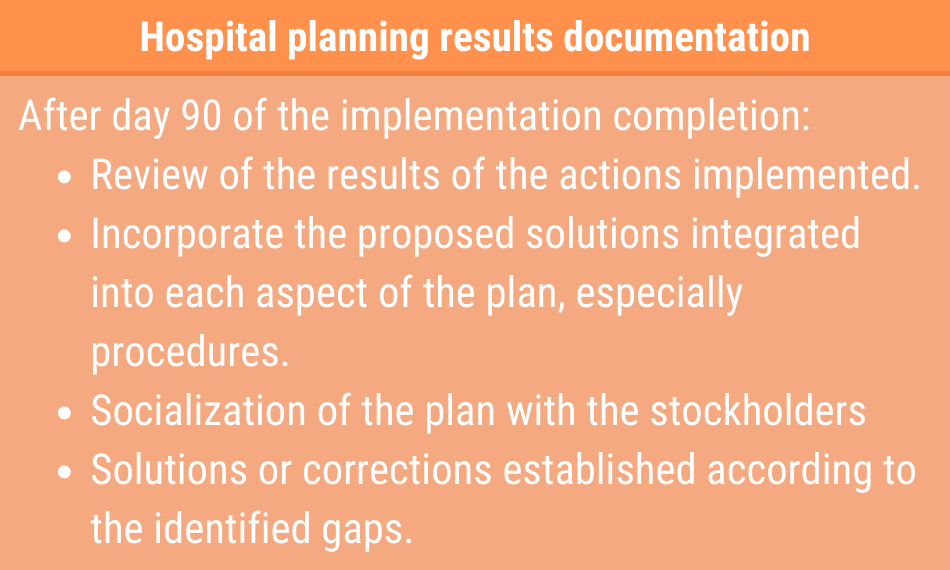
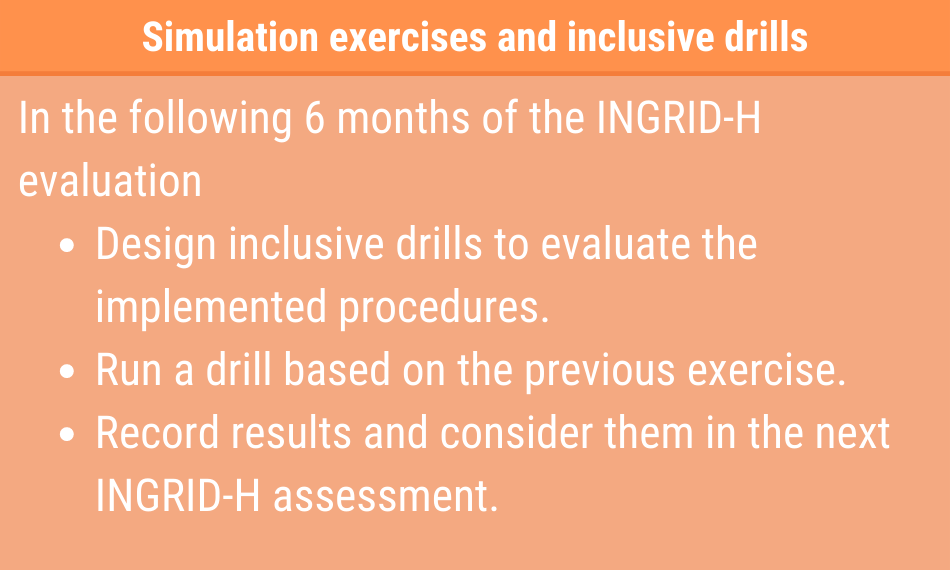
- Development and implementation of emergency risk reduction and management strategies for internally displaced populations (IDP), individuals with disabilities and countries in condition of high vulnerability.