Part IV
Survive, Thrive, Transform: Leaving No Young Person Behind in the Americas
IV.1 Introduction
This part of the document presents a forward-looking perspective on adolescent and youth health. It takes into account the lessons learned from the past as well as the evolving global and regional health developments and commitments, and their implications for the construction of a new adolescent and youth health agenda for the Region beyond 2018, when the current Action Plan comes to an end.
IV.2 The evolving nature of the adolescent and youth health agenda
The 2017 progress report on the Every Woman Every Child (EWEC) Global Strategy on Women’s, Children’s and Adolescents’ Health (149) states that until recently, adolescent health was a neglected topic. That report also notes that this has been changing, and has been reinforced with the recognition in the EWEC global strategy and other recent global documents that adolescents occupy a pivotal position in global public health and could play a transformative role within the 2030 Agenda for Sustainable Development (149).
IV.2.1 The global landscape
Major changes have taken place in the global landscape since the adoption of the Regional Strategy and the Plan of Action, including the sun-setting of the Millennium Development Goals and the adoption of the Sustainable Development Goals (SDGs), with a more ambitious and comprehensive agenda. In addition, the new Global Strategy for Women’s, Children’s and Adolescents’ Health puts adolescents and youth at the center of the SDGs, and central to achieving these goals. Further, new scientific and programmatic documents, such as the AAHA! (6) and the Lancet Commission report (3), make a strong case that investing in adolescents and youth is a requirement for development.
The Sustainable Development Goals
The 2030 Sustainable Development Agenda is of unprecedented scope and ambition (1). Poverty eradication, health, education, and food security and nutrition remain priorities in the SDGs. However, the goals also include a broad range of economic, social, and environmental objectives, offering the prospect of more peaceful and inclusive societies. The 17 goals and 169 targets include one specific goal for health: “Ensure healthy lives and promote well-being for all at all ages.” That goal has 13 targets (see Annex IV.A and Annex IV.B). There are many linkages between the health goal and other goals and targets (see Box IV.1). This reflects the fundamental assumption that health is both a major contributor to and a result of sustainable development policies.
In order to take on the wide range of crosscutting issues included in the SDGs, it will be necessary to achieve greater intersectoral coherence, integration, and coordination of efforts. This in turn will require strengthened local, national, regional, and global partnerships for sustainable development; a commitment to reach across sectors; clear and measurable objectives; and explicit attention to the needs of the most vulnerable and marginalized groups.
The Global Strategy for Women’s, Children’s and Adolescents’ Health
The 2016-2030 Global Strategy on Women’s, Children’s and Adolescents’ Health (2) builds on the previous Global Strategy on Women’s and Children’s Health (150), but explicitly, and for the first time, includes attention to adolescents. The Strategy focuses on three overarching objectives: 1) survive: end preventable deaths; 2) thrive: ensure health and well-being; and 3) transform: expand enabling environments. The Global Strategy aims to achieve these objective through a focus on the life course and evidence-based packages of interventions, as well as nine core action areas: 1) country leadership; 2) financing for health; 3) health system resilience; 4) individual potential; 5) community engagement; 6) multisector action; 7) humanitarian and fragile settings; 8) research and innovation; and 9) accountability for results, resources, and rights.
The Global Accelerated Action for the Health of Adolescents (AA-HA!) Framework
The 68th World Health Assembly requested that the WHO Secretariat develop a Global Accelerated Action for the Health of Adolescents Framework (“the Global AA-HA! Framework”) (6), in consultation with youth, Member States, and major partners.
The AA-HA! provides guidance to countries on how to plan, implement, and monitor a “survive, thrive, and transform” response to the health needs of adolescents, in line with the Global Strategy for Women’s, Children’s and Adolescents’ Health (2) and the operational framework for that Strategy (151), through:
- involving adolescents and the global health community in shaping its content and in setting a standard by which adolescents can help in holding countries accountable
- communicating evidence-based policies and interventions in health and other sectors for the “survive, thrive, and transform” agenda
- highlighting policies and interventions that address multiple outcomes, risk factors, and determinants and, therefore, give better value for money
- guiding priority-setting in various epidemiological contexts and providing options for implementation based on approaches that have been successfully applied in countries
- proposing tracer indicators for health and other sectors to monitor their performance vis-à-vis adolescent needs
The Committee on the Rights of the Child General comment No. 15
After the PAHO Regional Strategy and the Plan of Action were approved, the Committee on the Rights of the Child (CRC) published its “General comment No. 15 (2013): the right of the child to the enjoyment of the highest attainable standard of health (Article 24)” (152). This comment document does three things:
- highlights the underlying similarities between the scientific basis for a public health approach to adolescent health and a rights-based approach to health during the adolescent years
- outlines the normative content of the right of adolescents to the highest attainable standard of health and their right to facilities for the treatment of illness and rehabilitation in relation to health care services
- describes the legally binding obligations of States that are parties to the CRC with respect to ensuring the full realization of adolescents’ right to health, providing a conceptual framework and recommendations for concrete measures and actions required by States Parties, and non-State actors, to fulfill these obligations, and for developing the regular reports that they prepare for the Committee
In its “General comment No. 20 (2016) on the implementation of the rights of the child during adolescence” (153), the CRC provides guidance to States on the measures necessary to ensure the realization of the rights of children during adolescence. The issues highlighted in that document include:
- the importance of valuing adolescence and its associated characteristics as a positive developmental stage of childhood and the need to promote environments that help them to thrive; explore their emerging identities, beliefs, sexualities, and opportunities; balance risk and safety; build capacity for making free, informed, positive decisions and life choices; and successfully navigate the transition into adulthood
- that parental direction and guidance should be provided in a manner consistent with the evolving capacities of the child, and seeking an appropriate balance between respect for the evolving capacities of adolescents and appropriate levels of protection
- ensuring that all the rights of every adolescent boy and girl are afforded equal respect and protection and that comprehensive and appropriate affirmative action measures are introduced in order to diminish or eliminate conditions that result in direct or indirect discrimination against any group of adolescents on any grounds
- adopting measures that ensure that all adolescents have access, without discrimination, to different forms of media, and that support and promote equal access to digital citizenship, including through the promotion of accessible formats for adolescents with disabilities
- promoting safety of the digital environment through holistic strategies, including digital literacy with regard to online risks and strategies to keep it safe, and strengthen legislation and law enforcement mechanisms to tackle abuse online and fight impunity
- that all measures taken in respect of legislation, policies, and programs focused on adolescents should take into consideration intersecting violations of rights and the compounded negative effects on the adolescents concerned, in particular related to gender stereotypes affecting girls and boys; adolescents living with disabilities; lesbian, gay, bisexual, transgender, and intersex adolescents; and minority and indigenous adolescents
The report of the Lancet Commission on Adolescent Health and Wellbeing
A report published in 2016 by a special Lancet commission presented a series of landmark papers on adolescent health (3). This work brought together the most current evidence and insights from a network of global experts, including academics, policymakers, practitioners, young health advocates, and leading academic institutions representing diverse disciplines. The scholarly fields included public health and medicine, behavioral science, neuroscience, education, law, economics, and political and social science. Box IV.2 presents the key messages of the report.
Box IV.2: Key messages, opportunities, and challenges related to adolescent health, as presented by the 2016 report of the Lancet Commission on Adolescent Health and Wellbeing
Key messages
- Investments in adolescent health and well-being bring a triple dividend of benefits: now, into future adult life, and for the next generation of children.
- Adolescents are biologically, emotionally, and developmentally primed for engagement beyond their families. We must create the opportunities to meaningfully engage with them in all aspects of their lives.
- Inequities, including those linked to poverty and gender, shape all aspects of adolescent health and well-being. Strong multisectoral actions are needed to grow the resources for health and well-being and offer second chances to the most disadvantaged.
- Adolescents and young adults face unprecedented social, economic, and cultural change. We must transform our health, education, family support, and legal systems to keep pace with these changes.
Outstanding opportunities
- Guaranteeing and supporting access to free, quality secondary education for all adolescents presents the single best investment for health and well-being.
- Tackling preventable and treatable adolescent health problems (including infectious diseases, undernutrition, HIV, sexual and reproductive health, injury, and violence) will produce huge social and economic benefits. This is key to bringing a grand global convergence in health in all countries by 2030.
- The most powerful actions for adolescent health and well-being are intersectoral, multilevel, and multicomponent. Information and broadband technologies present an exceptional opportunity for building capacity within sectors and coordinating actions among them.
- Establishing systems for the training, mentoring, and participation of youth health advocates has the potential to transform traditional models of health care delivery to create adolescent-responsive health systems.
Challenges ahead
- Rapid global rises in adolescent health risks for later-life noncommunicable diseases will require an unprecedented extent of coordination across sectors, from the global to the local level.
- Noncommunicable diseases of adolescents (including mental and substance-use disorders, as well as chronic physical illnesses) are becoming the dominant health problems of this age group. Substantial investment in the health care system and approaches to prevention are required.
- Health information systems to support actions in adolescent health remain weak. Greater harmonization and broadening of data collection systems to neglected problems and younger ages will be needed.
- Inequalities in health and well-being are evident in socially and economically marginalized adolescents, including ethnic minorities, refugees, young offenders, indigenous individuals, and LGBT persons. Engagement of adolescents and reconfiguration of service systems to ensure equity of access regardless of sex, ethnic, or socioeconomic status will be essential.
Source: (3).
IV.2.2 The regional landscape
There have been a number of new regional commitments and developments that have implications for the health of adolescents and youth. Some of these were mentioned earlier in this report, including the regional commitment for universal health coverage and access (5), and the Plan of Action for the Prevention of Obesity in Children and Adolescents (124). Various other noteworthy regional products and commitments are highlighted below.

PAHO Strategic Plan for 2014–2019
The Strategic Plan of the Pan American Health Organization 2014-2019 is PAHO’s highest-level planning instrument, as approved by its Governing Bodies (154). The Plan prioritizes health equity, addressing social determinants of health, and Health in All Policies as strategic and cross-cutting approaches. The vision of the Plan goes beyond traditional disease-oriented approaches, and emphasizes health promotion, primary health care, and social protection in health as key tenets to realize healthy living and well-being for all citizens of the Americas.
The Panama Declaration on reducing inequities in reproductive, maternal, and child health
In September 2013, in the Panama Declaration on reducing inequities in reproductive, maternal, and child health (155), the Region renewed its commitment to improving the health of women, newborns, children, and adolescents, by reducing inequities, expanding evidence-based interventions, promoting universal health coverage, establishing regional cooperation mechanisms and partnerships, and mobilizing political will. In a follow-up to that Declaration, regional partners, including PAHO, UNICEF, the World Bank, the Inter-American Development Bank (IDB), and the U.S. Agency for International Development (USAID) established an interagency collaboration referred to as “A Promise Renewed,” with its Secretariat based at PAHO. Working collaboratively, the agencies took several actions to promote and support inequity analysis, including publishing a health equity report (156) and providing technical cooperation to countries to strengthen their capacity to conduct inequality analysis. Recently, A Promise Renewed transitioned into Every Woman Every Child Latin America and the Caribbean.
Addressing the causes of disparities in health service access and utilization by lesbian, gay, bisexual, and transgender persons
In recognition of the stigma and discrimination in the health sector against LGBT persons and the need to improve access to care and the overall health indicators for these populations, the PAHO Member States adopted the ground-breaking Resolution CD52.R6 in 2013 (157). The resolution urges Member States to: a) promote health services that respect human dignity and health rights, taking into account sexual and gender diversity; b) give priority to promoting equal access to health services in policies, plans, and legislation; and c) collect data about access to health care and health facilities for LGBT populations.
Within the context of this resolution, PAHO coordinated the implementation of an assessment on the health situation and access to care of LGBT persons, the barriers they can face in accessing health care services, and the impact of reduced access for this population (158). The findings are relevant to the situation of LGBT persons from all ages, including adolescents and youth. Key findings included that: 1) many countries that participated in the assessment have antidiscrimination policies in place and laws, policies and protocols tailored to meet the specific needs of LGBT persons, and health-related legislation includes laws that recognize LGBT groups as a population in conditions of vulnerability with unique health needs; however, some countries and territories still have laws that criminalize LGBT persons; 2) the provision of health services tailored to the needs of LGBT persons is heterogeneous in the Region. Most often, the services are offered through the public health system on an undifferentiated basis and are centralized in large urban settings, and stigma and discrimination continue to be major obstacles to access health services for LGBT persons (158).
In September 2017, the results of this assessment were presented to the PAHO Member States, with several recommendations, including the following: 1) Strengthen and/or establish LGBT-sensitive and comprehensive health services grounded in evidence that address the specific health needs of LGBT persons taking into account gender identity and diversity of expression; 2) Improve the training of health care providers so that they are able to address LGBT health needs with gender, diversity, and rights-based approaches that will help to end any form of discrimination; 3) Consider the specific health needs of LGBT persons in the development and/or implementation of health policies and health system strengthening initiatives as part of the effort to advance toward universal health; 4) Improve efforts to ensure that LGBT persons can enjoy access to and the use of health services without discrimination by including provisions in Member States’ national antidiscrimination laws that explicitly forbid discrimination on the basis of sexual orientation and gender identity; 5) Strengthen health information systems and surveillance mechanisms to generate periodic reports that include LGBT health conditions and barriers to access and include sexual orientation and gender identity items in existing nationally representative health surveys in order to gather data that can be disaggregated by sexual orientation and gender identity (158).
Montevideo consensus on population and development
Given the importance of sexual and reproductive health for adolescents, the Montevideo consensus on population and development (159) was a critical regional commitment made at the first session of the Regional Conference on Population and Development in Latin America and the Caribbean, held in August 2013. This document calls for investing in young people through specific public policies and articulates the regional commitment to effectively implement comprehensive sexuality education from early childhood; provide quality sexual and reproductive health services for adolescents and young persons that respond to their needs; introduce or strengthen policies and programs to prevent pregnant adolescents and young mothers from dropping out of schools; and eliminate unsafe abortions.
Health in All Policies
While not specifically aimed at adolescent and youth health, the Plan of Action on Health in All Policies, adopted by the PAHO Member States in September 2014 (Resolution CD53/10) (160), provided a framework for ongoing dialogue for and efforts toward multisectoral articulation of health improvement strategies. Such strategies are essential when it comes to the health of adolescents and youth, for example, when it comes to the food industry, efforts to reduce salt, fat and sugar contents, directly impact on the health of adolescents and youth.
Health, human security, and well-being
In 2010, PAHO Member States adopted a resolution titled “Health, Human Security, and Well-being” (CD50.R16) (161). The human security approach is based on fundamental human freedoms, including the right of people to live in freedom and dignity, free from poverty and despair (147, 161). Human security can serve as an overarching philosophy that aims to enhance human freedoms; can inform policy aimed at enabling individuals to fulfill their full potential; and can serve as a tool to guide practitioners in their programming aimed at reducing the sources of vulnerability facing individuals, communities, and institutions. In turn, human security can mitigate the impact of threats to people’s lives, livelihood, and dignity, and can build resilience to future threats (147, 161). The human security approach can contribute to programming related to the health and development of adolescents and youth, including in fashioning comprehensive approaches for reducing youth violence and promoting peace, development, and human rights.
The Commitment to Action of Santiago
In 2016, PAHO initiated action to roll out, in the Americas, the Global Strategy for Women’s, Children’s and Adolescents’ Health, in close partnership with other regional partners, including UNICEF, the United Nations Population Fund (UNFPA), the World Bank, the Joint United Nations Program on AIDS (UNAIDS), USAID, and IDB. Towards this end, an interagency coordinating mechanism was established, officially recognized by the EWEC global movement and named Every Woman Every Child Latin America and the Caribbean. The main purpose of the mechanism is to serve as a catalyst and to support countries in their efforts towards the goals and objectives of the SDGs and of the Global Strategy, with a focus on reducing health inequalities.
In this context, the interagency group organized several technical meetings and three subregional multisector stakeholder consultations (in the Caribbean, Central America, and South America). The objective was to disseminate the Global Strategy and to have in-depth discussions on its nine action areas during the first half of 2017. The reflections and recommendations generated by this regional consultative process served as input for a high-level meeting convened by Dr. Michelle Bachelet, president of the Republic of Chile and cochair of the High Level Advisory Group of the global EWEC movement. That event culminated in the Commitment to Action of Santiago (162), a regional pledge to ensure that every woman, child, and adolescent not only survives, but thrives in a transformative environment. This is to done by reducing health inequities, strengthening political will and multisectoral action, prioritizing quality, strengthening cooperation between countries, promoting a research agenda, investing needed resources, building participatory accountability mechanisms, and encouraging appropriate legislative frameworks.
The Sustainable Health Agenda for the Americas 2018-2030 (SHAA2030)
In September 2017, the Ministers and Secretaries of Health of the countries of the Region of the Americas unanimously endorsed the new health agenda for the Region, titled “Sustainable Health Agenda for the Americas 2018-2030: A Call to Action for Health and Well-being in the Region,” as the strategic policy instrument to provide direction and political vision for health development in the Region until 2030 (163).
The Agenda is based on the following principles and values: 1) the right to the enjoyment of the highest attainable standard of health; 2) Pan American solidarity; 3) equity in health; 4) universality; and 5) social inclusion.
SHAA2030 sets forth the following 11 health goals for the Region (163):
- Goal 1: Expand equitable access to comprehensive, integrated, quality, people-, family-, and community-centered health services, with an emphasis on health promotion and illness prevention.
- Goal 2: Strengthen stewardship and governance of the national health authority, while promoting social participation.
- Goal 3: Strengthen the management and development of human resources for health with skills that facilitate a comprehensive approach to health.
- Goal 4: Achieve adequate and sustainable health financing with equity and efficiency, and advance toward protection against financial risks for all persons and their families.
- Goal 5: Ensure access to essential medicines and vaccines, and to other priority health technologies, according to available scientific evidence and the national context.
- Goal 6: Strengthen information systems for health to support the development of evidence-based policies and decision-making.
- Goal 7: Develop capacity for the generation, transfer, and use of evidence and knowledge in health, promoting research, innovation, and the use of technology.
- Goal 8: Strengthen national and regional capacities to prepare for, prevent, detect, monitor, and respond to disease outbreaks, and emergencies and disasters that affect the health of the population.
- Goal 9: Reduce morbidity, disabilities, and mortality from noncommunicable diseases, injuries, violence, and mental health disorders.
- Goal 10: Reduce the burden of communicable diseases and eliminate neglected diseases.
- Goal 11: Reduce inequality and inequity in health through intersectoral, multisectoral, regional, and subregional approaches to the social and environmental determinants of health.
IV.3 Moving forward with the regional adolescent and youth health agenda
As the current Regional Strategy and Plan of Action on Adolescent and Youth Health are coming to an end, the recent global and regional developments presented in the preceding sections provide a sound basis for reflection and updating of approaches to improve the health and well-being of adolescents and youth in the Americas. There have been achievements and progress in the regional and country responses to adolescent and youth health, but major obstacles and challenges remain. In trying to apply the three-fold goal of the Global Strategy for Women’s, Children’s and Adolescents’ Health, there are three key challenges, as described below.
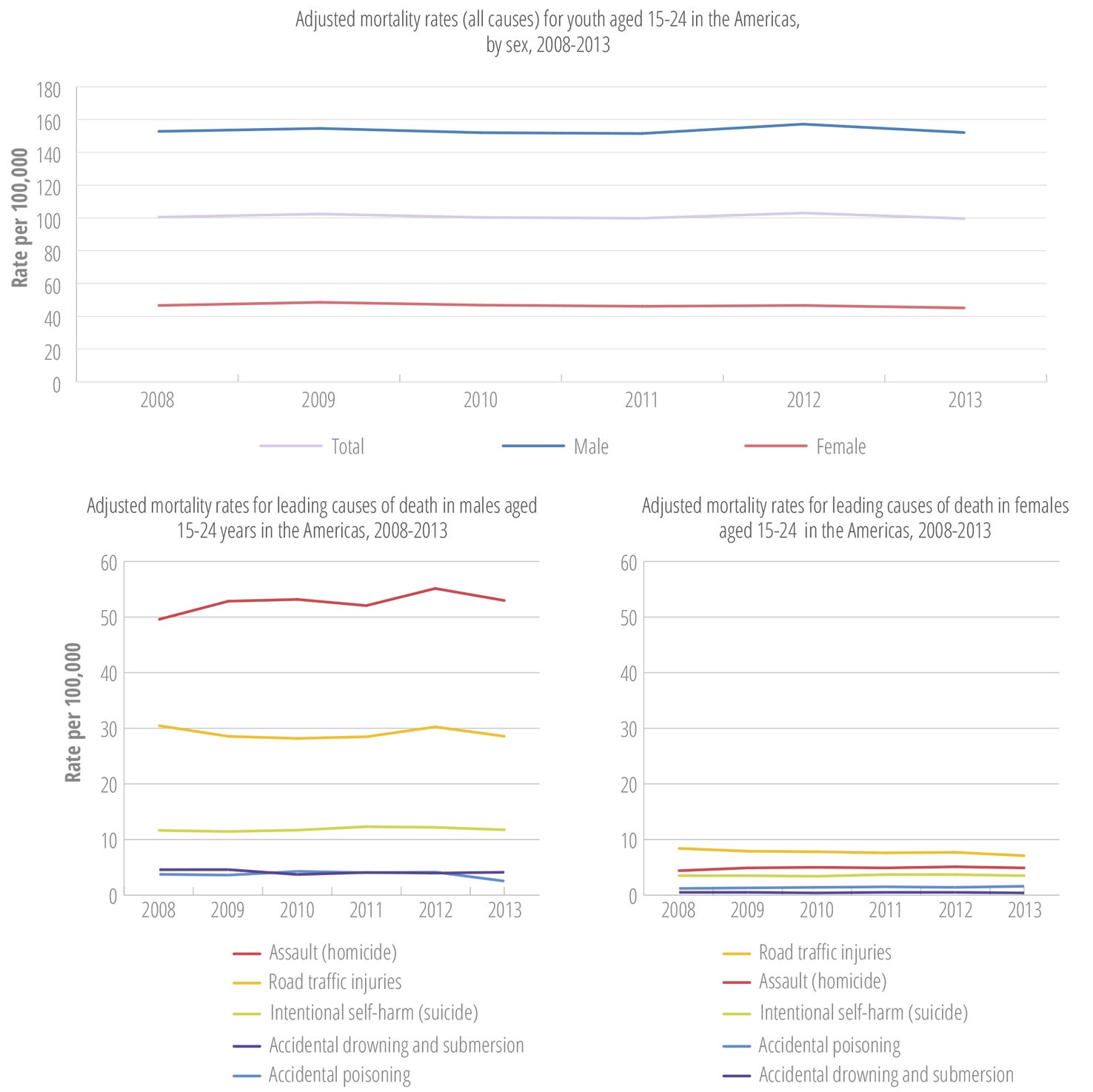
Survive
Adolescent and youth mortality rates have remained constant or have worsened, with young males dying, on average, four times more frequently than their female counterparts do. Each year more than 150,000 youth aged 15-24 years are dying in the Region. The majority of these deaths are due to preventable causes such as homicide, suicide, and road traffic injuries (Figure IV.1).
Inequality analysis shows that, in addition to gender, such social determinants as wealth quintile, education level, and race/ethnicity influence which groups are most affected by preventable mortality. Risk factors for mortality and morbidity during adolescence and youth, and into adulthood, such as alcohol and drug use, anemia, overweight and obesity, are highly prevalent. Further, there are only a limited number of comprehensive approaches in the Region that address these key risk factors contributing to youth mortality and morbidity, alcohol use, and mental health problems.
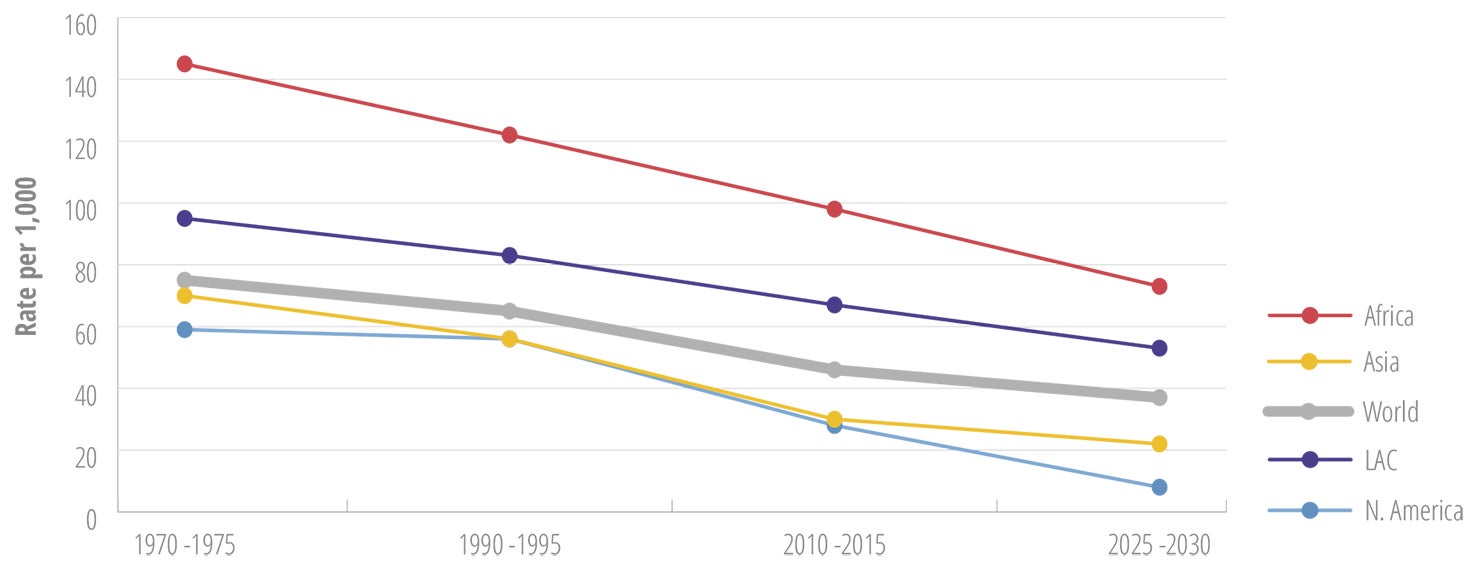
Thrive
The adolescent fertility rate in Latin America and the Caribbean remains among the highest in the world, with indigenous, rural, poor, and less-educated adolescent girls bearing the heaviest burden of early pregnancy (Figure IV.2). This affects their health and development opportunities across the life course and into the next generation. Nevertheless, adolescents continue to face major legal, policy, health system, and societal barriers to accessing sexual and reproductive services needed to manage their fertility and exercise their sexual and reproductive rights. Attention to the health of adolescents aged 10-14 years remains limited, thus missing the window of opportunity for early intervention and the fostering of positive and protective norms, values, and behaviors. Further, the focus of many programs and interventions remains on risk factors and deficiencies, with limited attention to fostering positive health and development of adolescents and youth.
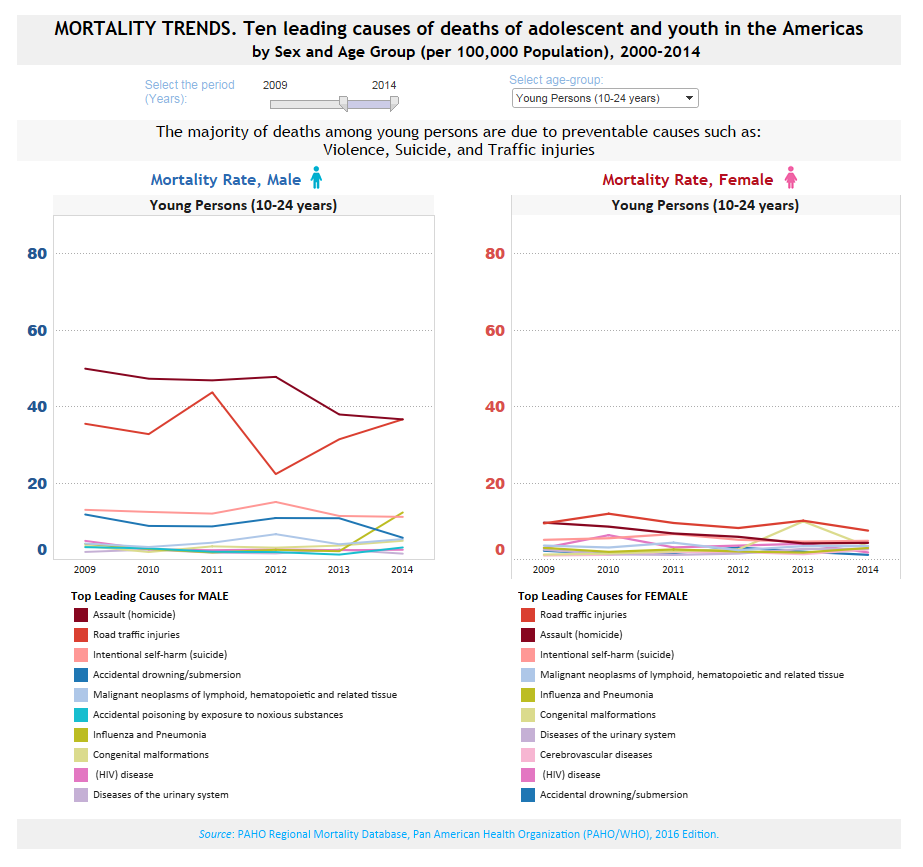
Data Visualization
MORTALITY TRENDS. Ten leading causes of deaths of adolescent and youth in the Americas, by Sex and Age Group (per 100,000 Population), 2000-2014
Transform
Many countries have low rates of secondary school completion, and young people in the Region continue to be disproportionately affected by poverty, unemployment, and inadequate access to decent employment. The health of adolescents and youth continues to be compromised by different forms of violence, including acts of aggression, sexual violence, neglect, and physical abuse, as evidenced by the rising homicide rates and the growing trend of pregnancy in girls under 15 years old. Meaningful engagement and participation of young people in efforts to improve their own health and development remain limited and incidental, rather than structural.
Proposed core elements for a 2030 adolescent health agenda for the Americas
To consolidate the gains of recent years and accelerate progress, the regional adolescent and youth health agenda must go beyond “business as usual.” To achieve the level of transformation envisioned by the SDGs and the Global Strategy for Women’s, Children’s and Adolescents’ Health, efforts will need to go outside the comfort zones of current adolescent health programs and address the complex health challenges young people face. These challenges include mental health problems and substance use, violence and suicide, and a range of health-related behaviors and conditions, including overweight and obesity. All of these problems have important implications for adolescent health and for public health across the life course. Fortunately, there is a growing evidence base for effective interventions to be implemented through the health sector and other sectors, to protect and promote optimal health and wellness of adolescents and youth. A future-oriented regional response to the health of adolescents and youth must include the following two core dimensions.
Reduction of preventable adolescent and youth morbidity and mortality, their risk factors and determinants, and the risk factors for premature adult mortality.
The mortality and burden of disease data indicate that the following areas should be prioritized to reduce adolescent and youth mortality and morbidity:
- a.Addressing youth violence and the factors contributing to perpetration or exposure to youth violence.
- b.Reduce the consumption of alcohol among adolescents and youth, including the early introduction of alcohol use.
- c.Promote and support the prevention, timely diagnosis and effective treatment of mental health challenges and diseases in adolescents and youth
- d.Promote healthy nutrition and actions to prevent anemia (in particular in young adolescents 10-14 years), and reduction of foods with high sugar and fat content.
Addressing the unfinished adolescent and youth mortality and morbidity agenda will require improvement of mortality reporting, as well as conducting additional analysis to better understand the circumstances of the leading causes of adolescent and youth mortality and the most affected groups. Based on this information, strategic actions should be developed and implemented, drawing from the lists of evidence-based interventions proposed by the WHO. Prevention efforts must apply multisector actions to address the underlying factors that contribute to preventable deaths among adolescents and youth.
Promotion of positive adolescent and youth health and development
The evidence base on the multiple-layer effects of interventions that apply positive development approaches is in line with longstanding global agreements, such as the Alma Ata Declaration (164), the Ottawa Charter for Health Promotion (165), the PAHO Strategy for Universal Access to Health and Universal Health Coverage (5), the SDGs (1), and the Global Strategy for Women’s, Children’s and Adolescents’ Health (2).
This second element concerns alternatives to traditional approaches that tend to be deficit based or focused on risk factors. Instead, there should be a positive developmental approach to adolescent and youth health that promotes constructive health and development by nurturing affirmative developmental assets. These assets include bonding, resilience, social and emotional and cognitive competence, self-determination, spirituality, self-efficacy, positive identity, and belief in the future. This approach aims to increase adolescents’ resilience and protective factors, and seeks to empower them to participate in a positive way in their own health, the health of their families, and the health of their communities (6). Key elements of these positive development approaches should include:
- Improving the use of the school platform for protection and promotion of the health and wellness of children and adolescents, to include 1) school health policies to promote and protect the health and safety of students; 2) fostering a healthy and safe learning environment; health education within and in addition to the school curriculum, and school-based health services.
- Working with families to maximize the health benefits of supportive and positive parent-child relationships.
- Working with the community to partner in the creation of the conditions for young people to be safe and healthy, and participate in society.
It is important to note that these two dimensions are not separate, but should rather be seen as inter-related, and parts of a comprehensive approach to achieve the “Survive-Thrive-Transform” adolescent and youth health agenda.
Proposed lines of action
Guarantee access for adolescents and youth to integrated and quality health services that are culturally, ethnically, and linguistically appropriate, with a gender approach, and promote health, prevent diseases, provide care for disease, and offer the necessary short-, medium-, and long-term care (5). This includes eliminating persistent barriers to access for adolescents, such as restricting laws and policies, and resistance based on cultural and religious arguments.
It is important to note that these efforts should go beyond the typical approach towards adolescent-friendly services (which tend to be small-scale and not sustainable), to the fostering of adolescent and youth-responsive health systems. This implies strengthening the capacity of existing health services to provide appropriate health services to adolescents and youth. Minimum requirements in this context are the development, institutionalization and continuous monitoring of standards for adolescent health services, definition and provision of an appropriate package of services, including SRH services, and training of health care providers in core competencies needed to provide services for adolescents and youth.
Implement evidence-based interventions in schools, families and communities for promotion and protection of health and wellness of male and female adolescents and youth.
- Efforts are underway for development of a blueprint for strengthening of school health, which will include consensus actions to address the mentioned aspects of school health, including renovation and expansion of school-based health services.
- Continued implementation and monitoring of the Familias Fuertes program, and introduction of other models of family-based programs.
- Articulation and implementation of a strategy for strengthening of positive health and development approaches in the Region.
- Strengthen stakeholder capacity to apply approaches in adolescent and youth health programs and services that will reduce inequities.
- Strengthening of monitoring and evaluation of programs, services and interventions, and sharing of lessons learned and good practices.
Continue building the regional and country-level capacity for the generation and use of strategic information related to the health and development of adolescents and youth, ideally as an integral part of the national health information system. This should include the generation of information on national and subnational levels, to include the health situation and risks, educational status, literacy, poverty, parental involvement, housing status, employment status, involvement with the justice system, perceived neighborhood safety, victimization of crime, and access to health care. Information on gender, sex, sexual orientation, gender identity, and gender equality should also be included and collected. Data need to be disaggregated based on a range of criteria in addition to age and sex, including socioeconomic status, education, ethnicity, rural/urban residence, and employment. This should include:
- Regular implementation of the Global School-based Health Survey (GSHS) and other surveys that generate data on the health and wellness of adolescents and youth.
- Strengthen stakeholder and capacity and support the measuring of health inequities affecting adolescents and youth.
- Promote and support implementation research to generate new knowledge on what works in the Region and to stimulate innovation.
Empowerment and engagement of adolescents and youth as partners and agents of change. Adolescents and youth can be powerful advocates and activists, and they can play key roles in program design, implementation, and monitoring. While this will clearly continue to be important, there is an ongoing need to be able to demonstrate how this involvement strengthens adolescent and youth health programs, and how young people can be more effectively integrated into national health systems as these systems move towards achieving universal health coverage.
Cross-cutting themes
Application of a life course approach: the main health challenges faced by adolescents do not take place in isolation, but are interrelated and influenced by what has happened during the first decade of life. Adolescent programs therefore need to link with and build on early child development (ECD) programs, which have changed to place greater emphasis on the relationships and environment of the child and the important role of caretakers and families. This building on ECD programs will require supporting close collaboration between child and adolescent health programs in countries. School health programs could play a critical bridging role in ensuring comprehensive and cohesive health services for children and adolescents across the life course. A life course approach also implies investing in encouraging healthy habits and a healthy environment for adolescents, to foster a healthier life trajectory and prevent health risks and conditions during adulthood.
Ensuring a rights-based approach: basing what is done on human rights emphasizes the commitments that Member States have made and the obligations that they have to implement interventions for adolescent survival and development. A rights-based approach provides a framework for national policies and legislation. Also, it stresses the importance of giving adequate attention to issues of equity and the engagement of adolescents, in particular those living in situations of vulnerability. There is a need to better use the existing conventions, treaties, and other legal instruments to influence the regional and country-level dialogue on the right to health of adolescents. This will require continued advocacy and support for legislative and policy reform based on human rights instruments and obligations, in order to ensure optimal access of adolescents to health information, services, and commodities, including those related to SRH.
Addressing inequities in adolescent and youth health: health inequities are the result of many factors, which are often interrelated. These factors include race, ethnicity, gender, sexual orientation, income level, place of residence, employment, and working conditions. Many health problems depend on social class, educational status, urban vs. rural residence, and ethnicity, particularly among indigenous groups and persons with a disability. It is therefore important for countries to assess indicators at subnational levels, to ensure that progress is made across the various subgroups of the populations of young people. A range of factors, from natural disasters to economic policies, may directly and indirectly affect the health of adolescents and youth. At the same time, subgroups of young people may become invisible in existing data collection systems and in the targeting of interventions. For example, young people with disabilities often remain unseen, with their special needs largely unmet. Identifying bottlenecks and reaching vulnerable and marginalized adolescents will require increased efforts if greater equity is to be achieved.
Tackling gender inequalities, including with more attention to young males: there have been significant efforts in the Region to direct resources to adolescent girls, particularly in the context of ASRH programs, and these need to be strengthened and taken to scale. There is, however, growing awareness of the need to also give adolescent boys adequate attention and to involve them more effectively. We must move beyond the false dichotomy of prioritizing men or women as if there is a competition, since the differential health care needs of both women and men must be met in order to achieve gender equality in health. The relational nature of gender implies that men and women are usually both affected by situations, events, and stressors, albeit in different ways. There is a need, in collaboration with regional partners, to develop and disseminate model interventions for involving men and boys in child and adolescent health.
Intersectoral collaboration: the major causes of mortality and of health challenges among adolescents and youth require interventions outside the health sector. Among these are road safety guidelines and measures; regulations related to alcohol and tobacco; food and nutrition policies; and protocols for responding to gang violence. Developing intersectoral and multidisciplinary partnerships will be essential, among government ministries (such as education and human development), the private sector, NGOs, community-based organizations, activists, parents, and young people themselves. The fact that this needs to be done is now widely accepted, but how to do it often remains challenging. There should be better documentation and dissemination of success stories, along with information on how success is assessed and achieved. There is an ongoing need to strengthen coordination between the UN and other partners and to facilitate joint support by development partners. This will help avoid competition and confusion, and also maximize the financial and technical resources for the benefit of national programs. Collaboration and exchange between countries to share successful experiences and approaches is also needed. Knowledge management within the Region will continue to be important so that countries can develop, review, and update national adolescent and youth health priorities, strategies, and plans, based on evidence and global and regional normative guidance. To this end, it will be important to document and share promising practices and to facilitate horizontal country-to-country exchanges.
Research and the use of new technology: there will always be a need for research on new approaches to improving adolescent health, but much is already known about effective interventions. A challenge for research is to focus less on answering “what” questions and more on addressing “how” questions. Operations research and implementation research will be important to provide real-time feedback during the implementation of adolescent health programs. Such research can help us better understand how effective programs were implemented, how they can be replicated in different contexts and for different target groups, and how they can be taken to scale while maintaining the quality that is required for them to be effective. An important intervention area that will require development and evaluation is the use of interactive media and social media. There is growing awareness of the potential benefits of m-health and e-health for reaching adolescents with information and education, linking them with services, and supporting adherence and follow-up. There is a need to collaborate with other partners to develop and disseminate model interventions for the use of digital media in relation to adolescent health.

