The All-in-One Telehealth Platform for NCDs program proposed by PAHO, which is part of the concept of a digital public good, is based on the provision of a comprehensive platform for the management of teleconsultations for primary health care with a special focus on NCDs.
Through this initiative, PAHO proposes to “accelerate” the implementation processes of telehealth programs, providing the software necessary for the integration of care between reference centers and primary care areas.
The program contemplates both asynchronous teleconsultation and synchronous consultation and enables the implementation of service models between patients and health teams and health teams among themselves (second opinion).
The platform implementation process proposes:
Provision of appropriate software in terms of interoperability and security for the comprehensive provision of telehealth services in accordance with the feasibility analysis carried out by the country/institution.
Technical cooperation for the implementation and adaptation to existing systems.
Support in the identification and definition of locations/institutions that have the necessary level of maturity to implement telehealth services in the defined period.
Support for the implementation of telehealth services focused on NCD care, as a starting point for the short-term incorporation of other services for remote health care, in its different modalities and in accordance with the regulations in force in the country.
Development of strategies, adjusted to local reality, to establish asynchronous telehealth services for collaboration between health teams (second opinion) based on the logic of integrated health service networks.
Support in terms of organizational change management and knowledge transfer to provide telehealth services under training and coaching strategies for health teams and resources for patient education.
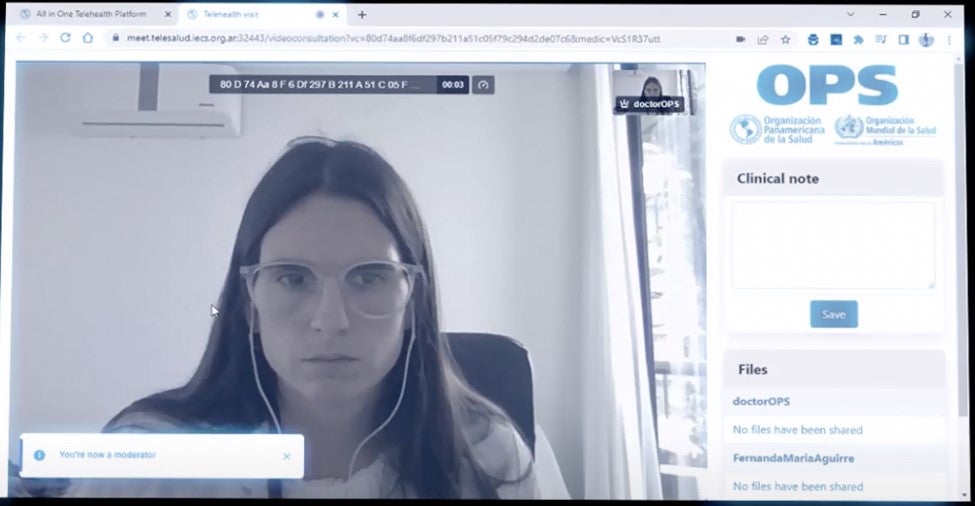
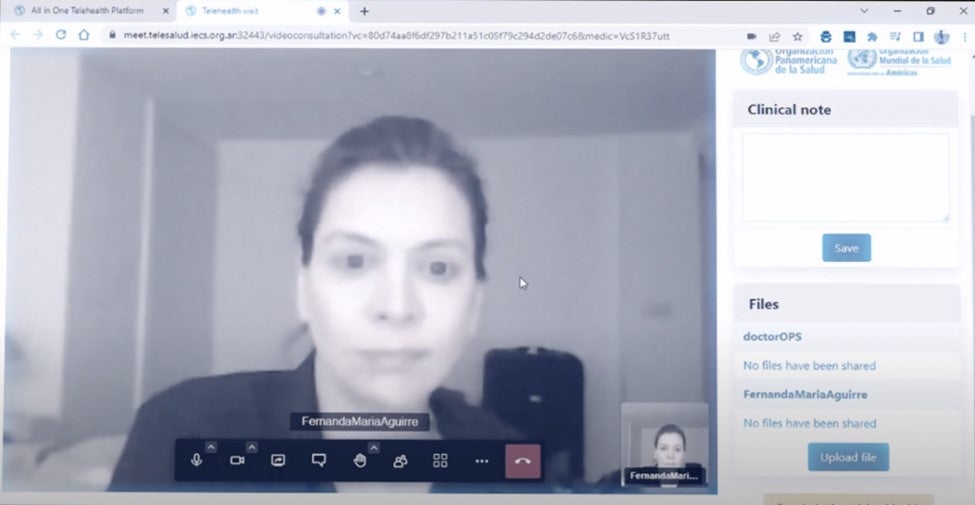
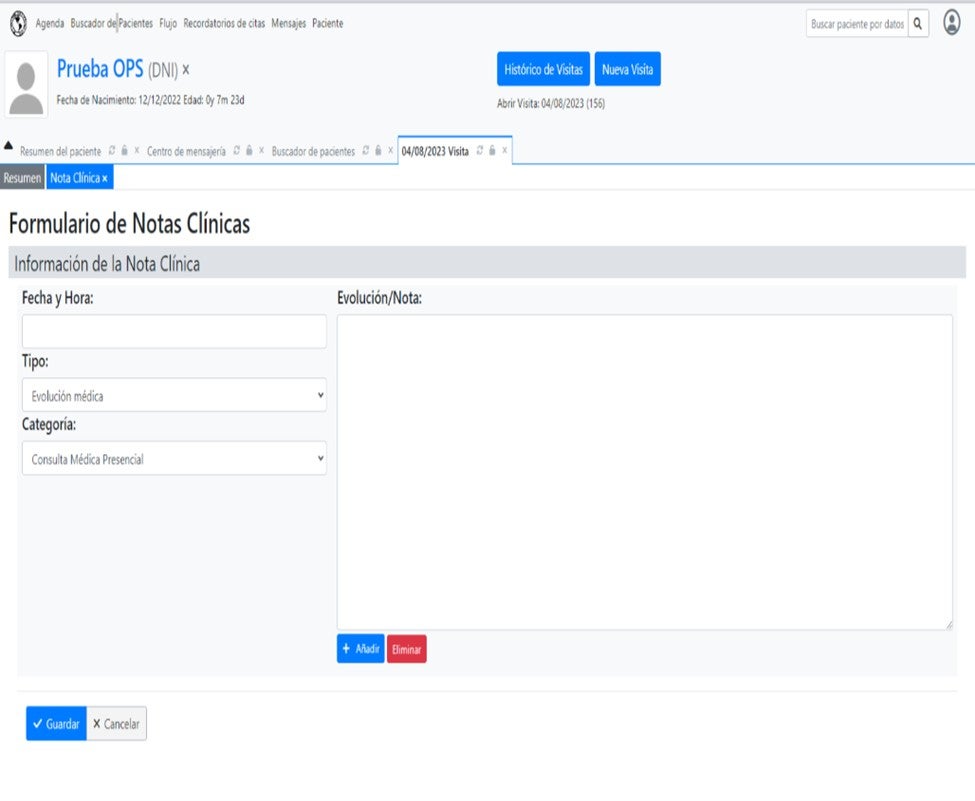
All-in-One platform: video consultation module
IO Standards
It is important to clarify that this platform will be able to integrate all patient information at the time of care and will have the capacity to share the information generated during the teleconsultation with the rest of the actors involved in the patient's care. In order to ensure the interoperability of these systems, it is based on international standards of syntactic and semantic interoperability.
The best-known international standards for the exchange of medical information, such as HL7, FHIR or DICOM, provide a common reference framework that allows the interaction and coordination of patient care. These standards offer uniformity in the naming of the components of the health system such as diagnoses, procedures, participants, interventions and the way they are transmitted, achieving interoperability between the various actors that interact with each other. In addition, they guarantee that the data in one part of the health system is available and meaningful not only across the variety of clinical and public health scenarios, but also at the administrative level.
Security and Quality
Data security and information quality are fundamental factors in the digital transformation process in health. Telemedicine is no exception to these generalities. Implementing platforms based on best practices not only guarantees people's privacy but will also strengthen trust in the system. The proposed platform was analyzed based on the highest security standards, such as the HIPAA standards in the United States or GDPR in Europe.
In order to facilitate the quality of information, the proposed software was analyzed based on concepts related to usability and ease of use, in order to optimize the time of professionals and achieve complete and as detailed clinical data as possible, which allows monitoring and control, that is, the continuity of care, of patients, especially vulnerable groups and patients with NCDs.
Telehealth Services
Synchronous or asynchronous model
Telemedicine services can be offered in two ways:
Asynchronous model: this is the model in which the person who consults and the person who answers are not online. It is generally implemented using structured forms where the request/clinical case is uploaded and answered in a scheduled time in an asynchronous manner. Sometimes files or images can be attached.
Synchronous model: the consultation occurs online, with people communicating live. It is generally implemented by teleconference service where audio and video are transmitted. Sometimes files or images can be attached.
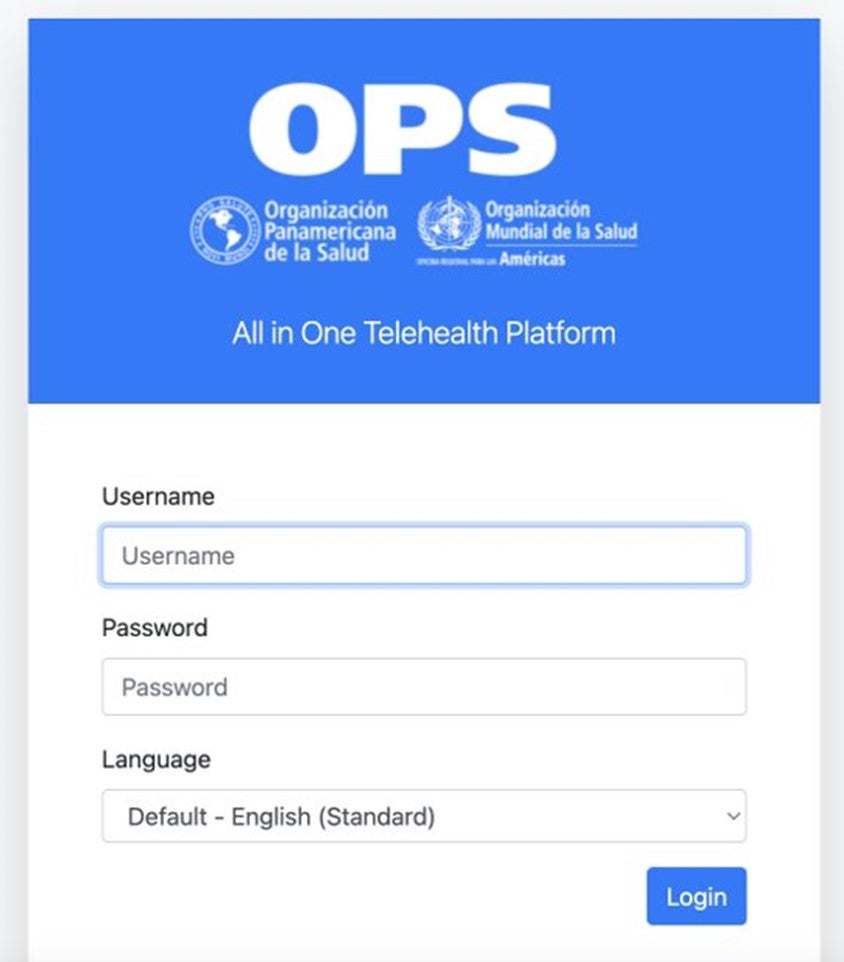
Login to the platform and clinical notes
Scheduled vs. Not scheduled
The difference in this case is whether the patient has a scheduled appointment to access the teleconsultation.
In the case of scheduled teleconsultation, the patient is assigned a day and time where he or she must connect to be seen by the health team.
In the case of unscheduled consultation, care generally occurs on a first-come, first-serve basis, which is commonly known as spontaneous demand. The patient accesses the service and remains on hold in line until someone from the health team is available to provide care.
Type of Services
Patient/health team is the care model that occurs between a patient or group of patients, or a patient and his or her family member/caregiver and someone from the health team. The main interaction is between the patient and the health team
Professional/professional | second opinion: is what we usually call a second opinion. It occurs between professional teams, generally in reference to a specific case, with or without the presence of the patient. The main interaction is between health teams.
Telemonitoring: This is a particular case, which can occur online or asynchronously, where a patient generally reports certain variables such as a vital sign or the evolution of a clinical condition. The most advanced telemonitoring models can integrate devices so that the patient does not need to transcribe said data. At the other end, a health team analyzes said data.
Implementation
PAHO proposes the telehealth program for noncommunicable diseases as a digital public good that is easy to implement and access.
The program, which includes the components described above, is delivered as a package of services that are “installed” on a server, parameterized according to local data, and can begin to be used.
However, the realities of each country or institution may be different, which is why we propose this implementation model on three levels:
1. Countries or institutions that do not have health information systems: implementation from scratch.
2. Countries or institutions with information systems, but that want to change: complete implementation and analysis of the data history for possible integration.
3. Countries or institutions with information systems, but that only want to install the teleconsultation module: adaptation and integration of specific modules.
Steps for All-in-One platform deployment.
Download all in one platform here: https://www.paho.org/en/information-systems-and-digital-health/paho-all…
Access to the manuals here: