HEATWAVES
Strengthening the capacities of the health sector and meteorological services to address heatwaves
Although heatwaves are not as destructive as other natural hazards, such as hurricanes and flash floods, they can cause mortality and morbidity that are not always immediately noticeable because of various causes, including the lack of surveillance systems for chronic diseases.
Heatwave negative health impacts are predictable and preventable via public health actions. Therefore, PAHO/WHO urges countries in the Americas Region to:
Strengthen health sector capacities and capabilities via the development of heatwave action plans comprising preparedness and response to this threat, and by doing this, prevent and reduce the excess of heat-related illness, deaths, and social disruption resulting from heatwaves.
Strengthen the capacities and capabilities of meteorological services to generate projections and predictions relevant to human well-being, and to promote close coordination between these services and the health sector, so that meteorological information is used for decision-making, before, during and after a heatwave strikes.
What is a heatwave?
What is the impact of heatwaves on human health?
What steps can people take to face a heatwave
What is the definition of heatwave?
According to the World Health Organization (WHO) and the World Meteorological Organization (WMO), there is no consensus on the definition of a heatwave. However, as an operational definition, they are understood as unusually hot, with either dry or humid periods during the day or night, which start and end abruptly, with a duration of two days or more and a discernible impact on human activities and natural systems.
How does the human body respond to heat?
The physiological response mechanism of the human body to heat includes an increase in body temperature. This increase in temperature is detected by the thermoreceptors, triggering the response of the thermoregulatory center, which reacts by activating peripheral vasodilatation and sweating. It activates the massive transport of blood to the periphery to facilitate cooling, causing an overload of the cardiovascular system. Excessive sweating, which can reach two liters per hour, causes a massive loss of fluids and electrolytes.
What are the determinants of vulnerability to a heatwave?
The major determinants of vulnerability of a population to temperature extremes relate to the features of the population exposed and their capacity to respond and adapt to the temperature conditions over long- and short-time frames. Determinants of vulnerability can be broadly categorized by demographic, health, physical, socioeconomic and institutional factors, many of which are inter-related and dynamic.
- Demographic determinants: The physiology of older people and the very young renders them more vulnerable to temperature extremes. They may also be less able to adapt their behaviors or environmental conditions and may be more dependent on others.
- Health status determinants: Many physical and mental health conditions increase vulnerability to adverse temperatures through a direct effect on the body’s physiology or through the effect of certain medications.
- Physical determinants: People spend approximately 80% of their time indoors, with the elderly or unwell spending longer periods indoors. Buildings (including homes, hospitals, schools and prisons) are not always adapted for temperature extremes and may have insufficient heating/energy efficiency or cooling measures.
- Socioeconomic determinants: People who are socially isolated are more at risk from temperature extremes because they are less able to access community support and may also have additional health or other vulnerabilities.
- Behavioral/cultural determinants: When temperatures become more extreme, most people take some action to adapt to the conditions. However, some factors limit the ability to adapt, such as age, poor health or economic circumstances, and certain belief or value systems may also mean that appropriate action is not taken in response to the temperature conditions.
- Institutional determinants: Health services need robust plans in order to manage the potential disruption and increased demand during and following temperature extremes; their ability to respond influences population vulnerability.
Source: Global Heat Health Information Network
What are the risk factors?
The major determinants of vulnerability of a population to temperature extremes relate to the features of the population exposed and their capacity to respond and adapt to the temperature conditions over long- and short-time frames. Determinants of vulnerability can be broadly categorized by demographic, health, physical, socioeconomic and institutional factors, many of which are inter-related and dynamic.
There are several risk factors that increase the effects of heat on human beings, as exemplified in Tables 1 & 2. Newborns, children and the elderly, as well as people with disabilities, those receiving medical treatment, and users of drugs and alcohol, are among the most vulnerable during heatwaves, and therefore can more easily develop adverse effects.
In addition, healthy individuals performing outdoor physical activities (work or sport) without taking protective measures, can also be affected.
Table 1. Health conditions that create high risk of health effects from heat
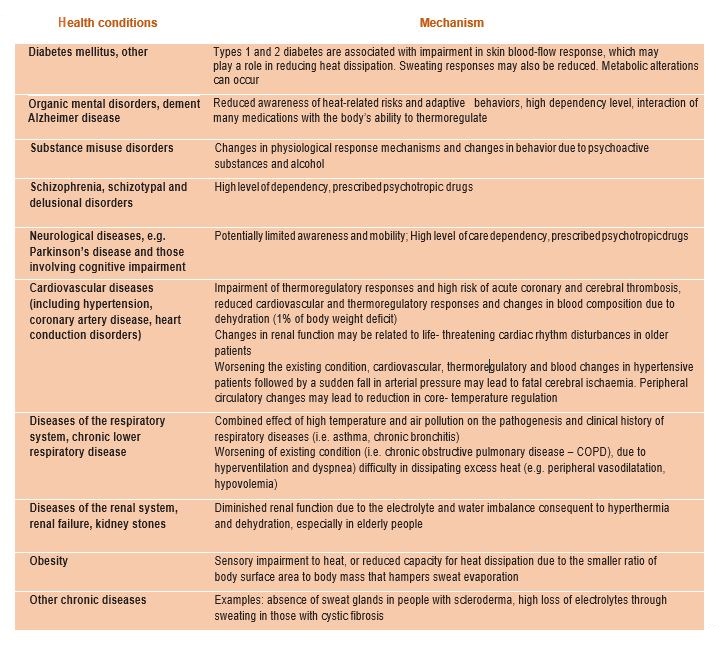
Source: Public Health Advice on Preventing Health Effects of Heat. WHO. 2011
Table 2. Adverse effects of medication during hot weather
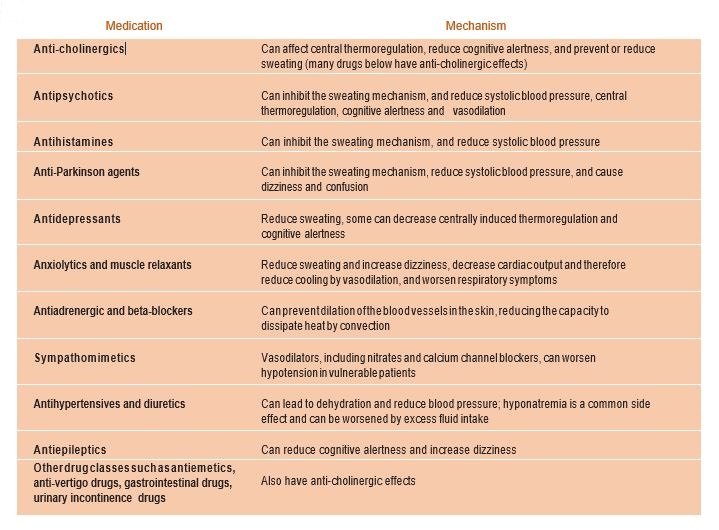
Sources: Public Health Advice on Preventing Health Effects of Heat. WHO. 2011. Adapted from Health Canada (2011b) and building on the work of Bouchama (2007), the National Centre for Diseases Prevention and Control (2011) and Hajat, O’Connor & Kosatsky (2010), National Collaborating Centre for Environmental Health (2011).
What are the effects of heatwaves on humans?
The scale and nature of the health effects and impacts observed depends on the timing, intensity and duration of the temperature event, the level of acclimatization and adaptation of the local population, infrastructure, knowledge and available equipment, the capacity and preparedness of the institutions to the response, as well as the definitions and methodologies , processes and procedures used. The precise threshold temperatures for health impacts vary by region and country, as does the scale of the health impacts by degree change in temperature, but the overall pattern remains similar.
For heat, deaths and hospitalizations occur extremely rapidly (same day) and they may be followed by a degree of impact displacement (health impacts in the frail brought forward), which returns to normal within a matter of days (Basu, 2009).
Exposure to heatwaves can cause edema, syncope, cramping, heat exhaustion and the feared heat stroke, that can lead to death. In addition, extreme heat can cause severe dehydration, stroke and contribute to the formation of clots. Few deaths are caused directly by heatwaves, while the majority are due to an exacerbation of cardiopulmonary, renal, and psychiatric diseases, due to heat.
Table 3. Definition of health effects due to heatwaves, signs and symptoms
Source: Public Health Advice on Preventing Health Effects of Heat. WHO. 2011
How strong is the effect of heatwaves compared to other natural disasters?
Although heatwaves are not as destructive as an earthquake or hurricane, they affect health, can cause the death, can generate damage in agriculture and livestock, and are often accompanied by power cuts, forest fires and droughts. As such they can affect food production, adversely affect livelihoods, and generate disruptions in the functioning of society. According to the National Environmental Information Centers of the National Oceanic and Atmospheric Administration (NOAA), in the last 30 years (from 1988 to 2017) heatwaves killed more people than other climate-related hazards in the United States of America.
Figure 1. Deaths caused by weather-related events in the United States of America (1988-2017)
What effects do the Heatwaves have beyond the health sector?
In addition to the impact on health, countries affected by heatwaves also suffered from power cuts due to an increased demand on energy supply for refrigeration (air conditioning), lack of water (drought or failures in the pumping), and lack of fuel. These caused the partial or total closure of financial services, health, water, commerce, schools, and transport. Some countries also reported shortages of fresh food (due to the breakdown of the cold chain and closing of the points of sale).
The risk of complex effects that a heatwave could generate require the participation of several instances related to risk management from a perspective of multiple threats. Therefore, the strengthening all sectors and key service providers through the civil defense system is needed, particularly in the areas of electricity supply, water supply, waste collection, transport, social services, first responders and public safety.
How has the behavior of heatwaves changed globally?
Historically, extreme heat events have occurred once or twice a year, with their effect being limited to a couple of countries and geographic areas within these countries. However, between the years 2000 and 2018, an increase in the magnitude, duration and intensity of heatwaves has been observed globally.
Between 2000 and 2016, the number of people exposed to heatwaves in the world has increased by at least 125 million, while the duration of the average heatwave is 0.37 days longer compared to the period 1986-2008. In 2015 alone, 175 million people were exposed to 627 heatwaves. (The Lancet Countdown on health and climate change: shaping the health of nations for centuries to come).
Figure 2. Percentile of temperatures on land and ocean, January to June 2018, registered by NOAA. Data source: GHCN-M version 3.3.0 & ERSST version 4.0.0
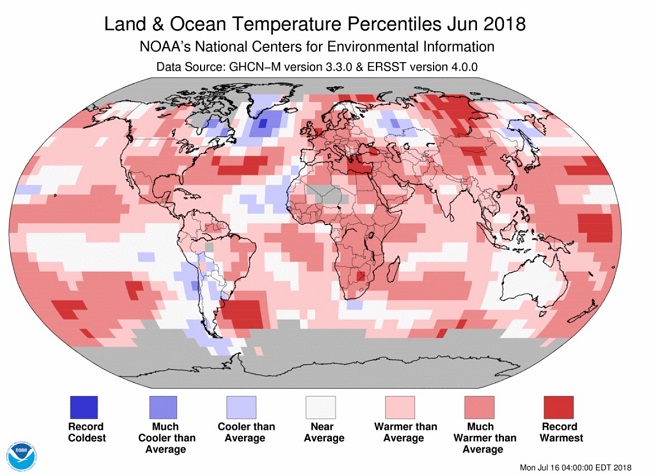
Source: NOAA, 2018
What are the most recent heatwaves that caused the most damage?
The mega heatwave that affected Europe in 2003 hit 16 countries and caused the death of at least 70,000 people. During this event 15,000 deaths occurred in France while 4,000 deaths occurred in the United Kingdom. This event confirmed the threat of heatwaves to life and health and emphasized the need for preparedness.
What was the human impact of heatwaves in the Americas?
The impact of heatwaves on human lives is unknown and due to the information available, any attempt to estimate it is an underestimation of the number of people affected. This is due to the lack of awareness of the problem, the lack of capacity to manage this threat by health personnel, the absence of operational definitions, the fact that health monitoring systems in countries do not look at deaths and disease caused by heat (with the exceptions of the USA, Canada and Mexico), the worsening of chronic diseases as a result of heat, and the inadequate coding of contributing conditions on death certificates.
To document the effects of heatwaves on health in the Americas, a review of news and reports available on the web was carried out. The analysis generated the following preliminary results, which need to be validated by the national authorities:
- The largest heatwave registered affected Argentina in 1900 and caused 478 deaths.
- More recently, heatwaves were recorded in:
o Brazil in 2010, mainly affected Rio de Janeiro and caused 735 deaths,
o Argentina in 2014, affected several provinces and caused 1877 deaths,
o Peru in 2016, due to El Niño-Southern Oscillation, caused the death of eight infants in Piura,
o Nicaragua in 2017, caused four deaths,
o Mexico and Paraguay in 2018 with 26 (7 more than in 2017) and four deaths respectively.
What happened in the region between 2018 and 2019?}
From the beginning of the Austral Summer in December 2018, six countries in the southern hemisphere declared a heatwave alert, plus one in the northern hemisphere, in the mid of the Boreal Winter. There are more countries affected but they did not declare an alert.
During the months of January and February 2019, the City and Province of Buenos Aires (Argentina) faced temperatures above 40oC.Hospitals, and health centers reported attending to patients with heat stroke, heat fatigue and associated diseases.
Meanwhile, during the month of January 2019, Paraguay registered temperatures between 30 and 43oC, resulting in the media attributed the deaths of two people to heat. In February, Uruguay registered a heatwave with temperatures above 40ºC. An increase in the number of visits to health facilities was reported, due to arterial hypotension, malaise, and decay. In Peru, temperatures were recorded above 33oC in Lima and 43oC, in the North with the possibility of high temperatures extending until April.
Meanwhile, in the northern hemisphere, Mexico had temperatures of up to 39oC in the Federal District and up to 45oC in Hidalgo.
What actions are proposed to enhance health sector preparedness while facing a moderate or severe heatwave?
Health sector strengthening actions should seek to strengthen governance, preparedness and response, by developing contingency plans from a multiple-threat perspective, that includes the characterization of the threat, roles and functions, activation and deactivation procedures, and institutional coordination. The elaboration of these plans requires a mapping of risks, vulnerable population, available capacities, capacities, and resources.
The activities of the national plan should be aimed at strengthening or developing capacities for surveillance of morbidity and mortality associated with extreme heat and related causes in the epidemiological surveillance systems, strengthen meteorological early warning mechanisms with Meteorological Services and its coordination with the health sector, train human resources at all levels, strengthen the response capacity of health facilities in areas of greater risk and vulnerability, and provision of equipment (also include fans , air conditioning, batteries and solar panels or generators) and supplies.
Local authorities should know what concrete actions they are able to carry out to mitigate the effects of the heatwave including the heat island effect in urban environments (via the implementation of community cooling centers), the coordination of local resources for the response, and actions to reduce temperatures in poor households, health services, schools, and nursing homes. The population component should be oriented to inform about the threat, risk factors, and what to do if someone has symptoms caused by heat or chronic diseases that were aggravated by heat.
In case a heatwave interrupts basic services, or occurs concurrently with a fire, drought, flood, tornadoes, or epidemic, it is necessary to work with civil defense and the actors responsible for the response.
Who does climate and weather monitoring?
The monitoring of heatwaves is carried out by Meteorological Services. Based on this monitoring the Meteorological Services issue forecasts and/or predictions, including heatwaves alerts.
The weather monitoring systems are based on meteorological variables (e.g. maximum and minimum temperatures, humidity, winds). The Meteorological Services also preserves historical records and has the capacity to project and model based on historical data, following the WMO guidelines.
What is a heatwave alert?
A heatwave alert is a communication from the Meteorological Services and the Ministry of Health, informing the government authorities and population about the occurrence of a heatwave in the immediate future (3 to 5 days before) or mediate future (1 to 3 months). As these heatwaves may have implications for health, an intervention may be required to prevent negative impacts on health. It is important that the alert is issued before the heatwave begins to reduce the associated mortality, particularly in vulnerable populations.
Are Member States prepared to face a heatwave?
The threat of heatwaves is different from other threats and requires specific preparations and capabilities. While the progress achieved in emergency and disaster preparedness may contribute to the response to mild heatwaves, these may not be enough if the region is affected by moderate or severe events, such as those that affected Europe in 2003 and Russia in 2010.
According to the International Panel for Climate Change (IPCC) projections, more frequent heatwaves will become hotter, start earlier, and last longer in the coming years, so that the Ministries of Health and the National Meteorology and Hydrology Agencies must be prepared.
EL NIÑO-SOUTHERN OSCILLATION
El Niño and La Niña are climate patterns in the Pacific Ocean that affect weather worldwide. During normal conditions in the Pacific Ocean, trade winds blow west along the Equator, taking warm water from South America towards Asia. To replace that warm water, cold water rises from the depths — a process called upwelling.
El Niño and La Niña are two opposing climate patterns that break these normal conditions. Scientists call these phenomena the El Niño-Southern Oscillation (ENSO) cycle.
El Niño and La Niña both have global impacts on weather, wildfires, ecosystems, and economies. Episodes of El Niño and La Niña typically last nine to 12 months, but can sometimes last for years; they typically start around April and peak in intensity between November and February of the following year. El Niño and La Niña events occur every two to seven years on average, but they don’t occur on a regular schedule. Generally, El Niño occurs more frequently than La Niña. Read more
El Niño is typically associated with below normal rainfall in Central America from July to December and in northern parts of South America from June to March.
WHO Public Health Situation Analysis: El Niño
El Niño conditions increase the probability of a range of extreme hydro-meteorological events, including droughts, floods, hurricanes, and heatwaves, all of which are detrimental to human health.
The ongoing El Niño is highly likely to have wide-ranging health implications on a global scale well into 2024. In the coming months, the most severe health risks are likely to arise from malnutrition due to ongoing food insecurity, compounded by the effects of El Niño. Other very high risks include cholera and other waterborne diseases; heat stress and air pollution; malaria; and arboviral diseases such as dengue, Zika virus disease, and chikungunya.
Central America and northern South America - high-risk countries are part of the sub-regions identified as high priority for potential humanitarian challenges due to the consequences of El Niño through September 2023. These high-risk countries are Colombia (northern region), El Salvador, Guatemala, Guyana, Honduras, Nicaragua, Peru (northern region), Suriname, the Bolivarian Republic of Venezuela (northern region).
El Niño-Southern Oscillation: a call to action for public health emergency preparedness and response
In 2023, El Niño notably affected health infrastructure in various countries, particularly in South America. In nations such as Peru and Ecuador, health facilities underwent significant physical damage due to El Niño
The public health implications of the ongoing El Niño- Southern Oscillation (ENSO) events in 2023 are significant. The primary health consequences related to El Niño, such as malnutrition, heat stress-respiratory diseases, vector and waterborne diseases, direct injuries and fatalities, disruption of health services, and mental health effects, among others, should be broadly addressed considering local contexts and vulnerabilities, with a multi-hazard management approach.
This initiative is being implemented collaboratively between the Departments of Health Emergencies (PHE) and Social and Environmental Determinants for Health Equity (DHE).