To effectively meet the needs of the population, health
services must be integrated, accessible, and acceptable and must provide continuous, comprehensive care. PAHO Member States have undertaken major efforts to reorganize their health systems with these objectives in mind, following the principles and elements of primary health care. In 2008–2009, this work ranged from sweeping decentralization efforts to more focused initiatives aimed at improving the quality and acceptability of care. PAHO provided important support for these efforts through its technical cooperation in the countries, as highlighted below.

In Argentina, PAHO promoted a perinatal care program at the Ramon Sarda Mother-Child Hospital as a model for transforming conventional maternity centers into family-centered maternity services. The program seeks to put expectant and new mothers and their babies at the center of their families through such measures as including family members in prenatal checkups, encouraging them to accompany mothers during labor and delivery, allowing fathers and other family members into neonatal support units, facilitating skin-to-skin contact between babies and their mothers, and providing mothers of hospitalized infants with access to special lodging and meals, with volunteers providing care. PAHO produced a publication presenting the program as a “best practice,” citing such indicators as a neonatal death rate of less than 2 per 1,000 (excluding babies with lethal defects and those weighing less than 750 grams) and a 90 percent usage rate for the special lodging and meals. PAHO also facilitated on-site training at the R. Sarda hospital for multidisciplinary teams from other facilities, as well as later visits by R. Sarda health professionals to those same facilities for reinforcement and follow-up.
Also in Argentina, PAHO supported the consolidation of the country’s National Nursing Development Plan, aimed at increasing the number of nursing professionals and training nursing aides. The initiative emphasizes nursing skills needed in primary health care and is being applied in 42 nursing schools, with the goal of increasing the nursing workforce to 45,000 by 2016.

PAHO’s Country Office in Belize is supporting efforts to integrate HIV prevention, care, and treatment as well as prevention and control of chronic noncommunicable diseases into primary health care. These include efforts to reduce stigma and discrimination as a barrier to effective HIV intervention, as well as support for the development of protocols on diabetes, hypertension, nutritional management, and physical activity for use in primary care settings. In a related effort, PAHO in early 2009 collaborated with the Belize Diabetes Association to provide training to community-based health personnel in foot care for people with diabetes. Plans are in progress for follow-up training in Jamaica.
PAHO has also supported efforts in Belize to strengthen community mental health services in the context of primary health care. PAHO’s technical cooperation supported capacity building for psychiatric nurse practitioners, development of a mental health policy, development and use of a mental health training manual for police officers, and drafting of a plan for mental health in disasters. Concomitantly with these efforts, Belize has reduced the number of psychiatric hospital admissions and has increased the number of mental health outpatients.

In Bolivia, PAHO worked in 2008 with the Ministry of Health and Sports to provide graduate-level training for doctors using a new conceptual model called Community, Family and Intercultural Health. The training incorporated the principles of primary health care and focused on the experiences of first-level care in rural and urban areas. The student physicians are expected to eventually hold positions in management and delivery of services at the level of health networks, and the training equips them to improve service delivery and to advocate efforts to address the determinants of health among local authorities.
In Brazil, PAHO has been supporting the formation of multidisciplinary teams to provide people-centered family health care as part of the country’s Family Health Strategy. By early 2009, more than 230,000 health workers in 30,000 teams were providing services to an estimated 50 percent of the population across the national territory. In areas where the strategy is not yet implemented, primary care services are being provided through a more traditional services-on-demand approach. However, this model is being gradually supplanted by the Family Health Strategy.
PAHO also supported the incorporation of a clinical Pharmaceutical Assistance Model into Brazil’s Family Health Strategy as part of larger efforts to strengthen policies on rational use of drugs and essential supplies. In addition, PAHO has supported the QualiSUS Project, which is strengthening the health services infrastructure of Brazil’s health networks.
PAHO’s Country Office in Chile worked with the Latin American Center for Perinatology and Human Development (CLAP) to develop a country-to-country technical cooperation project promoting maternal, neonatal, and child health. The project was the first line of action of the “Let’s Act Now for Mothers and Children” launched in September 2008 by Chilean President Michelle Bachelet. The project will be carried out in Bolivia, Ecuador, and Paraguay.
Also in Chile, the PAHO/WHO Collaborating Center for Primary Health Care, in the School of Nursing at the Pontifical Catholic University of Chile, developed an innovative program to provide “distance care” via telephone for patients with diabetes and other chronic conditions. The program, ATAS–UC (Spanish acronym for Telephone Support for Self-Care in Health–University of Chile) focuses especially on self-management for patients with diabetes type 2.
In Colombia, PAHO supported the Ministry of Social Protection’s efforts to expand coverage and strengthen the model of care for tuberculosis patients in eight departments with high proportions of indigenous people. The care model is based on the principles of primary health care and includes specific intercultural approaches for each ethnic group. A central aim is to gain acceptance from the indigenous population through intercultural dialogue and the participation of indigenous organizations as leaders and effective channels for communication and implementation of actions in health. A new investment of US$500,000 will facilitate the expansion of the model to an additional 15 ethnic groups.
Also in Colombia, PAHO supported the design of a model for providing child health services in areas with little access to health care or high concentrations of displaced people, where infant mortality rates are high. The model provides curative and preventive health care through mobile teams, with costs absorbed by the country’s social security system. In a related effort, PAHO is working with health authorities, insurers, and providers to apply the Integrated Management of Childhood Diseases (IMCI) strategy to achieve comprehensive care for pregnant women and children under 5 in the three provinces of Colombia’s “Coffee Belt.”
In Cuba, PAHO has focused its technical cooperation on consolidating the country's notable achievements in primary health care. In 2008–2009, PAHO worked with the Ministry of Health to strengthen municipal health departments and the nearly 500 polyclinics that provide preventive and curative care services throughout the country. So far, more than two thirds of the polyclinics have benefitted from new equipment and personnel training in areas including sonography, radiography, endoscopy, opthamology, optometry, rehabilitation, urgent care, laboratory capacity, and information systems. PAHO also helped strengthen the National Health System’s statistical network and health surveillance system to support situation analysis for primary health care.
In the Dominican Republic, PAHO has supported the development of a network of regional health services, including the rehabilitation and construction of new health centers, acquisition of equipment, and needs evaluations to ensure that population demands can be met. PAHO also supported efforts to strengthen human resources for primary health care through the training of 55 national- and regional-level facilitators who in turn will train health professionals in first-level care. Other Dominican health professionals are taking courses through PAHO’s Virtual Campus in Public Health.
PAHO helped organize the first Eastern Caribbean Conference for Health Services Managers and Clinical Engineers, in October 2008, which brought together hospital administrators, health services managers, clinical supervisors, and clinical engineers from 10 countries to share state-of-the-art information about health systems development, technology management, and clinical engineering. PAHO is also supporting training on management of diabetes and hypertension for health teams and other health partners.
In El Salvador, PAHO supported improvements in the quality of health services in metropolitan San Salvador through the strengthening of providers’ capacities and skills, and through the provision of basic equipment for perinatal care. PAHO also supported the reorganization of family and community care with a participatory focus, including the empowerment of women and involvement of other sectors besides health.
PAHO’s Faces, Voices, and Places regional initiative provides leadership for primary health care renewal by modeling health promotion interventions that address the social determinants of health. The initiative was conceived to showcase efforts to advance the Millennium Development Goals (MDGs), especially those related to health, in the poorest and most vulnerable communities of Latin America and the Caribbean. The specific interventions are based on an analysis of local realities and are being developed and carried out by the communities themselves with technical assistance from PAHO and other agencies of the United Nations system.
Activities during 2008 in two towns in El Salvador illustrate the initiative’s promotion of primary health care through an intersectoral, multiprogrammatic approach to integrating health services. In 2008, PAHO helped carry out participatory local health assessments (diagnósticos) in the towns of Rosario de Mora and Santiago Texacuangos, in the country’s south. The work included situation analyses, identification of problems, and support for the design of local health plans based on the new vision of primary health care, with a focus on reducing inequities and extending social protection using a family health model. The assessments were carried out with the active participation of local residents and all sectors involved in health, under the leadership of the Ministry of Public Health and Social Assistance and the municipal governments.
Similar work is being carried out as part of the Faces, Voices, and Places initiative in more than 30 communities in 17 countries of the Region (see box). The initiative also supports MDG-promoting interventions in Guyana and Haiti through a PAHO–European Community partnership and has shared its tools and methodologies for participatory research and community capacity-building with Argentina, for its Healthy Municipalities Network, and with Colombia, which is promoting healthy environments and intersectoral alliances in 100 of its most vulnerable communities.
PAHO is working with the Hospitals Cooperative of Antioquia, Colombia (COHAN), a PAHO/WHO Collaborating Center for Essential Drugs and Hospital Supplies, to promote a new tool for improving health services management known as PERC (from the Spanish for “production, efficiency, performance, and costs”). The effort includes the development of manuals and virtual courses as well as training for managers and other users. PERC builds on and replaces the WinSIG information management system, also developed by PAHO.
In Honduras, PAHO helped the Civic Council of Popular Indigenous Organizations (COPINH) develop the Utopia Center, which serves as a “meeting and friendship center” for the Lenca community of La Esperanza, Intibucá. It will serve as a venue for training and capacity building in areas including natural and traditional medicine, sustainable agriculture, alternative credit and savings, integrated farming, gender issues, and solutions to health problems that affect indigenous people. The center, funded by the Lydia Behm trust, includes a museum on Lenca culture, a library, a radio transmitter, a study and computing area, a kitchen, an administrative area, and four dormitories. The 7-hectare compound also has a fruit grove and vegetable garden.

PAHO’s Latin American Center for Perinatology and Human Development (CLAP) produced and disseminated new Guidelines for the Continuum of Care of Mothers and Newborns in the Context of Primary Health Care, along with a series of practical manuals, training materials, and other publications covering such subjects as perinatal infections, utilization of the Perinatal Information System, family planning, and child health promotion. During 2008–2009, the center organized 30 workshops in 12 countries, training more than 800 participants from throughout the Region in maternal and child care. It also supported long-distance training courses on community and clinical application of the Integrated Management of Childhood Diseases (IMCI) strategy, covering such areas as case management, health promotion, organizational skills in the delivery of appropriate care, and key family practices in hard-to-reach and vulnerable areas.
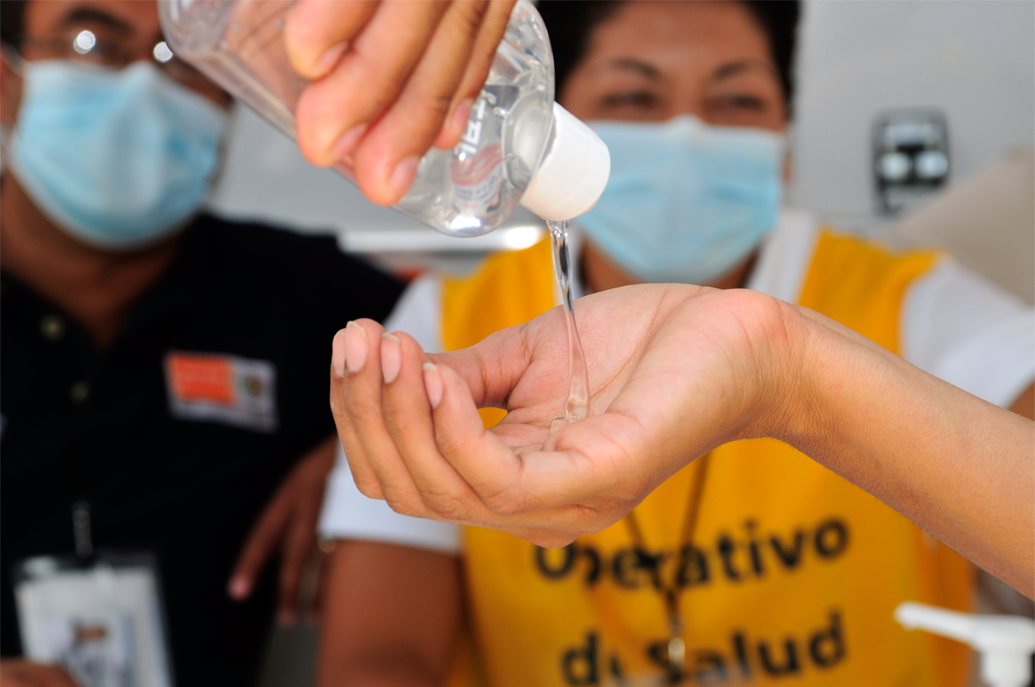
Since before the start of the H1N1 influenza pandemic, PAHO provided technical cooperation to Member States in Latin America and the Caribbean to foster an efficient response from the primary health care services in the event of a pandemic. As part of pandemic preparedness efforts, PAHO provided specific recommendations on preparing health facilities for unusual or unexpected cases of acute respiratory illness and guidelines on case identification and triage of patients with respiratory symptoms, with emphasis on the need for early detection and reporting of unusual cases.
Following the outbreaks, PAHO produced and disseminated a technical document on the primary health care strategy and the response to the pandemic, which encourages a comprehensive, integrated approach that focuses not only on hospitals but on all levels of care, that facilitates family and community participation in prevention and home care, and that involves other sectors, including educators and faith-based groups.
PAHO also provided specific recommendations and training on infection control in health facilities and helped countries throughout the Region procure personal protective equipment for health workers, with special support for lower-income countries. PAHO also provided guidelines on clinical management of cases, risk communication for health service managers, the organization of health services in countries where the virus has and has not yet been reported, and responding to a second emergency (such as a natural disaster) during an influenza pandemic.
PAHO is also working to ensure equitable access for its Member States to antiviral drugs and vaccines for novel H1N1.
PAHO carried out a number of initiatives in 2008–2009 targeting communicable diseases that also helped to strengthen primary health care in Member States.
PAHO supported the implementation of an Integrated Management Strategy for the Prevention and Control of Dengue (EGI-dengue) in member countries, with a strong focus on primary health and environmental care. Strategies developed for Bolivia and Chile, and currently under development for Puerto Rico and the Caribbean, address the disease at all levels of patient care, with emphasis on primary care, which offers the best opportunities to prevent deaths from the disease. Among the goals in these strategies is to have 100 percent of health units in each country using established standards for dengue care.
PAHO collaborated with the Department of Health in Chiapas, Mexico, to develop an integrated action plan for the control and elimination of neglected infectious diseases (onchocerciasis, trachoma, Chagas’ disease, and leishmaniasis) with a focus on primary health care services and improved water supply.
PAHO collaborated with the Department of Health in Chiapas, Mexico, to develop an integrated action plan for the control and elimination of neglected infectious diseases (onchocerciasis, trachoma, Chagas’ disease, and leishmaniasis) with a focus on primary health care services and improved water supply.
PAHO is also carrying out a number of efforts centered on tuberculosis treatment and control that serve to strengthen primary health care. These include efforts to improve comprehensive care of patients with TB through training of health workers in HIV testing and counseling and in health education for patients, the family, and the community, and through better clinical management of the disease; the promotion of community participation in the DOTS strategy; strengthening of laboratory networks; capacity building for management of medicines; training in basic epidemiology; and work with the public and private sectors to incorporate service providers into the network of primary health care services.
PAHO continued its support for efforts to scale up and reorient health services for HIV prevention and care based on the principles of the renewed primary health care strategy. An important initiative was the insertion of comprehensive HIV care into curricula for nursing, psychology, and medical schools in the Andean Region. The program also adapted specific HIV modules from the Integrated Management of Adult Illnesses (IMAI) strategy for use in Latin America and the Caribbean, organized a three-day regional discussion with national AIDS and tuberculosis program managers on enhancing comprehensive services for HIV and TB treatment and control, and produced interim guidelines for TB/HIV care and related training modules, job aids, and posters for health care providers.
PAHO also worked in 2008–2009 to raise awareness of the effectiveness, feasibility, and safety of the “screen and treat” approach to cervical cancer in primary health care. PAHO has helped implement the approach in Guatemala and Peru, and began similar work in Paraguay as part of an integrated primary health care package. PAHO also worked with the Ministry of Health in Nicaragua to train providers and improve the quality and coverage of cervical cancer screening services in primary health care.
In Nicaragua, PAHO supported an evaluation effort by the Ministry of Health that assessed progress and challenges in the implementation of health policies based on primary health care. Through a process known as JABA, evaluations were carried out in 149 of the country’s 153 municipalities. They identified a number of major advances including the provision of free health services, improvement in the provision of medicines in the ministry’s health units, the development of special health days and health fairs, and non-denial of requested services. The JABA process is designed to enhance public accountability.
Also in Nicaragua, PAHO supported the implementation of a Family and Community Health Model in 11 departments to improve the delivery of health services and to expand immunization coverage in remote communities. As part of these efforts, PAHO worked with the Ministry of Health to strengthen supervision of immunization services at all levels, to evaluate the quality and capacity of the cold chain, to introduce the new pneumococcal vaccine, and to support the decentralization of antiretroviral treatment to 23 health establishments.
In Panama, PAHO helped the Ministry of Health develop and disseminate new guides for comprehensive care for patients with diabetes, obesity, and hypertension. The guides, which are part of Panama’s renewed primary health care strategy, promote prevention and control of these conditions in first-level care settings, with a focus on community participation.
In Peru, PAHO has provided support for decentralization of the health system, strengthening of primary care, and efforts to ensure universal access to health.
Peru’s decentralization efforts have transferred 125 functions of the health system from the central level to the departmental level. To support this process, PAHO has provided technical cooperation for the organization and development of health services based on the principles of primary health care, with a focus on such areas as referral and cross-referral systems, accreditation of services, guaranteed quality, planning, and financing. In addition, PAHO has helped develop a new family health strategy aimed at expanding health services and strengthening primary care with an emphasis on prevention and health promotion, particularly for low-income people. In implementing the family health strategy, Peru has reoriented its health care model from a focus on comprehensive care for individuals to comprehensive family care.
PAHO is helping Member States improve the quality of health services through a regional initiative to improve the health and safety of health workers. Highlights of this initiative in 2008–2009 included an effort to vaccinate 1.5 million health workers in Peru against infectious diseases acquired through occupational transmission, including hepatitis B.

In Suriname, PAHO is supporting a Health Sector Plan that aims to improve health coverage, strengthen primary care, and improve the efficiency, equity, and quality of health services. As part of this support, PAHO has participated in a Community Primary Health Care Steering Committee that conducted a rapid assessment of existing health services in the interior, to serve as the basis for the introduction of comprehensive and integrated health services delivery throughout the country’s health system. PAHO is also collaborating with UNICEF and the United Nations Population Fund (UNFPA) to introduce comprehensive primary health care through an integrated management approach in 57 clinics that are part of Suriname’s private, faith-based Medical Mission network. With adaptations, the approach is expected to become the national standard for primary clinics in the public sector as well. In addition, PAHO has helped adapt algorithms and protocols from the Integrated Management of Childhood Diseases (IMCI) approach to Suriname’s particular needs and standards.
In Trinidad and Tobago, PAHO has supported a primary health care approach through the promotion of integrated delivery systems and the integration of mental health services into community-based primary health care. PAHO helped organize three initiatives in these areas: a National Forum on Mental Health Promotion and Mental Disease Prevention and a National Consultation on Integrated Delivery Systems, both in October 2008, and a workshop on Strengthening the Mental Health System in March 2009. The consultation on Integrated Delivery Systems provided feedback for a PAHO regional proposal on integrated delivery systems that grew out of the process of renewal of primary health care.
As part of its support for health reform in Uruguay, PAHO helped develop a training program on primary health care that hopes to reach 3,000 physicians from both the public and private sectors and from throughout the country. PAHO’s country office developed the curriculum for the program, with the participation of public and private institutions, including the University of the Republic of Uruguay. The goal is to provide a professional reorientation for the participants so they can better respond to the demands of a primary health care–based system. PAHO has also promoted similar activities in other departments.
Also in support of health reform in Uruguay, PAHO helped carry out a pilot project on primary oral health care in the department of Canelones. The project promoted use of the Atraumatic Restorative Treatment (ART), a procedure for removing dental caries with hand instruments, which can be used by nondental personnel and primary health care workers. The pilot project carried out sociological and anthropological studies to assess local community oral health conditions and needs, including a survey using the DMF (decayed, missing, filled) index, which allows for comparisons of the oral health of different groups and across countries.
In the Turks and Caicos Islands, PAHO provided training in contact tracing and counseling for nurses and medical practitioners caring for HIV/STI patients. PAHO also provided support for an assessment of the island’s mental health services, utilizing the WHO’s Assessment Instrument for Mental Health Systems (WHO-AIMS). The findings are being used to develop a draft mental health plan that will focus on primary health care.
PAHO in 2008 provided support for Venezuela’s Barrio Adentro (“Inside the Neighborhood”) initiative, which has installed 8,000 “consultation points” in people’s homes and has constructed 3,580 clinics whose main priority is care for low-income people who have traditionally lacked access to rural and urban health services. The initiative has led to the expansion of primary health care to some 17 million people throughout the country and has formed the basis for the creation of Comprehensive Community Health Areas as operating units for the health system, providing health care in conjunction with local governments and the citizenry.
Also in Venezuela, PAHO supported efforts to incorporate a Plan of Universal Access to Treatment for Tobacco Dependency into the National Public Health System, through a network of primary care facilities. The initiative has trained 1,125 doctors, nurses, psychologists, and psychiatrists. Between July 2008 and February 2009, the initiative reached some 3,000 smokers, with a smoking cessation rate of 16 percent at the end of treatment. The cost-free treatment includes the use of bupropion and nicotine patches.

In late 2008, PAHO’s Virtual Campus in Public Health offered its first course on capacity building for the renewal of primary health care, and 59 students from 17 countries in the Region completed the course.
In Puerto Rico, PAHO began discussions with the Department of Health to establish a node of the Virtual Campus of Public Health at the School of Public Health of the University of Puerto Rico. PAHO recently assigned five virtual rooms of the campus to work in coordination with the university.
PAHO worked with a C$12 million grant from Canada through the Canadian International Development Agency (CIDA) to promote an integrated and intersectoral approach to communicable diseases, with emphasis on reducing inequities in access to health services and addressing the priority health needs of vulnerable and marginalized populations. The program targets selected areas in Colombia, Ecuador, Paraguay, and Peru and follows the principles of primary health care, with special emphasis on community disease surveillance, health promotion and education, and building local capacity to increase community participation and empowerment.
In addition, during 2008–2009 PAHO worked with nearly €2 million from the Government of Spain to improve the organization, management, and delivery of health services in Latin America and the Caribbean as part of efforts to reduce illness, disability, and premature mortality in the Region. The funds supported efforts to strengthen organizational and management capacity in health institutions and health service delivery networks, based on the principles of primary health care, as well as improvements in primary care and promotion of policies and strategies for integrating health services networks. The funds also supported efforts to strengthen emergency medical services; the development of a regional strategy to improve safety and quality of care, including the establishment of a Regional Observatory on Patient Safety and Quality of Care; efforts to fight chronic noncommunicable diseases in the Caribbean and elsewhere; and efforts to improve screening and treatment for cervical cancer in Bolivia, Haiti, and Paraguay.
PAHO helped organize the first Regional Colloquium on Organization and Management of Emergency Health Services, held in Medellin, Colombia, in November 2008. The meeting brought together experts from Argentina, Brazil, Costa Rica, Colombia, Chile, Mexico, Panama, Peru, Spain, Trinidad and Tobago, and the United States to develop collective lines of action for improving emergency health services throughout the Region. Discussions covered issues such as legal frameworks for health policy, organization and management of pre-hospital care, emergency room management, human resources and equipment for emergency services, and emergency medical services and disaster response. Participants in the colloquium pledged to form a team of experts to help PAHO design a regional strategy for strengthening emergency medical services in the Americas.
One of PAHO’s most important technical cooperation initiatives during 2008–2009 was the development of recommendations for integrating health care delivery networks, including public and private providers, as a primary health care–based solution to the fragmentation of health systems. The initiative is based on evidence that poorly integrated health services are a major cause of weak health system performance, resulting in inefficient use of resources, poor quality of services, lack of continuity in care, high costs, and low user satisfaction.
Fragmentation is closely related to, and partly the result of, institutional segmentation, in which different subsystems provide health services for different groups depending on their ability to pay or their employment status (public or private sector employee or unemployed). Segmentation produces fragmentation when the infrastructure and capacities of these subsystems are not coordinated or integrated. Fragmentation can also result from other trends, including the decentralization of health services without adequate coordination of levels of care; the prevalence of programs focused on specific diseases, risks, or population groups; overspecialization and overemphasis on curative rather than preventive care; poor organizational models; and the proliferation of “vertical” and other narrowly focused programs funded by international donors and cooperation agencies. Symptoms of fragmented health systems include low rates of case resolution at the first level of care, the use of emergency services to obtain specialized care, the hospitalization of patients who could have been treated on an outpatient basis, and extended hospital stays because of difficulties in discharging patients who lack social support.
To address these problems, PAHO developed a proposal for a regional policy on integrated health services delivery networks (IHSDN), defined as networks of organizations that provide-or make arrangements to provide-comprehensive health services to a particular population and that are willing to be held accountable for their clinical and economic outcomes and the health status of the population they serve. The concept allows for contractual arrangements or strategic partnerships between different providers, including public and private (and even in different countries), that offer complementary services. The networks can be based on a number of models, provided they meet a few key requirements, including having:
A “roadmap” for developing IHSDN throughout the Region was presented to the PAHO Executive Committee in June 2009 for consideration by the 49th Directing Council in September–October. PAHO has formed partnerships with the Ministry of Health of Brazil, the German Agency for Technical Cooperation (GTZ), the Hospital Consortium of Catalonia (Spain), and the Hospital Cooperative of Antioquia (Colombia), and is seeking additional partners to support the initiative.